Apocrine hidrocystoma of the orbit mimicking basal cell carcinoma: a case report
Slim Werda, Racem Choura, Ahmed Chebil, El Ouafi Alexandre Bouazzaoui, Leila El Matri
Corresponding author: Racem Choura, Department B of Ophthalmology, Hedi Rais Institute of Ophthalmology, Tunis, Tunisia 
Received: 02 Jun 2020 - Accepted: 02 Nov 2022 - Published: 03 Nov 2022
Domain: Ophthalmology
Keywords: Apocrine, hidrocystoma, orbital cystic mass, case report
©Slim Werda et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Slim Werda et al. Apocrine hidrocystoma of the orbit mimicking basal cell carcinoma: a case report. PAMJ Clinical Medicine. 2022;10:25. [doi: 10.11604/pamj-cm.2022.10.25.23966]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/10/25/full
Apocrine hidrocystoma of the orbit mimicking basal cell carcinoma: a case report
Slim Werda1,2, ![]() Racem Choura1,2,&, Ahmed Chebil1,2, El Ouafi Alexandre Bouazzaoui1,2, Leila El Matri1,2
Racem Choura1,2,&, Ahmed Chebil1,2, El Ouafi Alexandre Bouazzaoui1,2, Leila El Matri1,2
&Corresponding author
Apocrine hidrocystomas are benign cystic lesions derived from the sweat glands. They are rarely seen in the orbit with very few adult cases published in literature. We present a case of a 40-year-old female, with no prior medical history or ocular trauma, referred for an orbital tumor. We found a raised, pearly, blue-grayish and painless mass, medial to her left upper eyelid, in the supero-medial orbit margin. The diagnosis of a basal cell carcinoma was suspected, and a complete excisional biopsy was performed. Histopathologic examination revealed apocrine hidrocystoma. Apocrine hidrocystomas, although rare, should be part of the differential diagnosis of orbital cystic tumors at any age. Our aim was to emphasize the resemblance of apocrine hidrocystoma to basal cell carcinoma.
Apocrine hidrocystomas are benign cystic lesions derived from the sweat glands. They are typically located on the face, particularly in the eyelid margins. Apocrine hidrocystomas are rarely seen in the orbit. Only very few cases in adults have been published in literature [1-4]. We present a case of a 40-year-old female, with no prior medical history or ocular trauma, referred for an orbital tumor.
Patient information: a 40-year-old female patient, presented in October 2019, with a bluish tumor of the inner canthus of the left eye. No history of ocular trauma was reported.
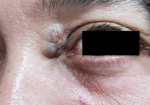
Clinical findings: on inspection, the lesion was bluish-gray, 10 mm in diameter, with a warty and pearly appearance, located in the internal canthus facing the lacrimal sac. It was firm and painless on palpation (Figure 1). The patient´s eye movements were unrestricted. There was no associated skin disorder, no neurological deficit or changes in visual acuity or optic nerve function.
Timeline of current episode: August 2009: the lesion appeared, and a scan has concluded to a cystic origin. A simple marsupialization of the cyst was performed. January 2016: First recurrence, a puncture was made. October 2019: Second recurrence. Due to the failure of previous treatments, the patient was referred to us.
Diagnostic assessment: the diagnosis of a basal cell carcinoma was suspected, and an excisional biopsy was indicated.
Therapeutic interventions: the excision of a skin spindle next to the tumor showed that the lesion is not cutaneous, but rather subcutaneous. We made a progressive dissection releasing the tumor from the surrounding tissue, then an enucleation and hemostasis (Figure 2). Finally, the skin has been sutured. The excised lesion was sent for histopathologic examination.
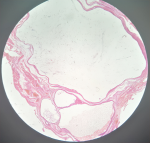
Follow-up and outcome of interventions: macroscopically, the mass was 10x7x0.5 mm in size, it contains a cyst, filled with fluid, of 8 mm long axis without any endo or exokystic vegetations. Histologically, the tumor presented a multilocular cyst with several juxtaposed cystic cavities. They are lined by a vascular and fibrous tissue wall composed by a double epithelial cellular layer. An outer layer composed of cubic flattened cells, and an internal thicker layer composed of secreting cylindrical cells, having an eosinophilic cytoplasm with a characteristic decapitation secretory apical prominence. The results of the pathologic analysis reported that the mass was consistent with apocrine hidrocystoma with no histological signs of malignancy (Figure 3).
Patient perspective: “I was scared. I thought I had cancer. Pathology results were a great relief for me.”
Informed consent: the patient gave written informed consent for surgical procedure and scientific participation.
The orbital location of apocrine hidrocystoma is extremely rare, as indicated by the few cases described in the literature, mainly after trauma [1-4]. Hidrocystomas are classified according to the type of secretion: eccrine or apocrine [1,5,6]. Both types can be found on the face, but the apocrine type is less likely to be in the periorbital area [1,7]. Hidrocystomas in the periorbital region are often located in the eyelid and inner canthus [6]. Aprocrine hidrocystomas tend to be darker, larger and solitary. Multiple forms are rare and may be an important marker for some rare inherited diseases [8,9]. Although benign, hidrocystomas may cause functional impact (closing of the palpebral slit and compression of the lacrimal duct), esthetic burden and psychological distress in patients [9]. The benign differential diagnosis of solitary apocrine hidrocystoma includes eccrine hidrocystoma, epidermoid or pilar cysts. The malignant tumor that may have a similar clinical presentation are mainly melanoma and basal cell carcinoma [8]. Our patient had a raised, pearly, firm, blue-grayish and slow-growing lesion that could be mistaken for a basal cell carcinoma. The pigmented appearance may be due to the presence in the cystic fluid of lipofuscin pigments [8]. The diagnostic confirmation is histological, but it may be suspected clinically. In our case, we performed a surgical excision, which is the only approach that allows the practitioner to carry out both the final diagnosis and the treatment of these tumors. A few years earlier, our patient had a needle puncture; however, local recurrence is frequently observed with this treatment. In the literature, no cases of spontaneously involuting apocrine hidrocystomas have been reported [8].
Orbital apocrine hidrocystoma may mimic a basal cell carcinoma and, although rare, should be considered in the differential diagnosis of cystic mass of the orbit in any age group.
The authors declare no competing interests.
Slim Werda wrote the manuscript. Racem Choura revised the manuscript. Ahmed Chebil was involved in the clinical and therapeutic management of the patient. Leila El Matri is responsible for the overall scientific management. Racem Choura and El Ouafi Alexandre Bouazzaoui finalized the manuscript. All the authors read and approved the final version of manuscript to be submitted for publication.
Figure 1: preoperative photography of the tumor: bluish-gray, with a warty and pearly appearance, located in the internal canthus of the left eye facing the lacrimal sac
Figure 2: preoperative photography: skin incision, dissection of the subcutaneous tissu, dissection of the tumor mass, and mass removal
Figure 3: histological confirming: multilocular cyst with several juxtaposed cystic cavities
- Valenzuela AA, Heathcote JG. Apocrine hidrocystoma of the orbit. Orbit. 2011;30(6):316-317. PubMed | Google Scholar
- Mehta A, Rao A, Khanna A. Sudoriferous cyst of the orbit of adult origin after trauma. Indian J Ophthalmol. 2008;56(3):235-237. PubMed | Google Scholar
- Rosen WJ, Li Y. Sudoriferous cyst of the orbit. Ophthalmic Plast Reconstr Surg. 2001;17(1):73-75. PubMed | Google Scholar
- Ferraz LB, Burroughs JR, Satto LH, Natsuaki KL, Meneguin RLFS, Marques MEA et al. Three Adult Cases of Orbital Hidrocystoma Presenting with Blepharoptosis. J Clin Med. 2015;4(1):150-158. PubMed | Google Scholar
- May C, Chang O, Compton N. A giant apocrine hidrocystoma of the trunk. Dermatol. Online J. 2017;23(9):13030. PubMed | Google Scholar
- Marangoz D, Doğan Ekici I, Çiftçi F. Orbital Eccrine Hidrocystoma. Turk J Ophthalmol. 2016;46(5):251-254. PubMed | Google Scholar
- Sarabi K, Khachemoune A. Hidrocystomas-a brief review. MedGenMed. 2006;8(3):57. PubMed | Google Scholar
- Jakobiec FA, Bhat P, Kropp TM. Palpebro-orbital apocrine cystadenoma: immunohistochemical verification of a unique variant with a critical differential diagnosis. Ophthalmic Plast Reconstr Surg. 2010;26(4):245-249. PubMed | Google Scholar
- Suimon Y, Kase S, Ishijima K, Kanno-Okada H, Ishida S. Clinicopathological features of cystic lesions in the eyelid. Biomed Rep. 2019;10(2):92-96. PubMed | Google Scholar