Lipoma of the vallecula: a rare cause of upper aerodigestive tract obstruction (case report)
Bonko Neville, Acha Everistus, Ghislain Feudjio, Brandon Carl Monika, Chin Virginia, Nantang Marleens, Nyoma Nancy
Corresponding author: Bonko Neville, Cameroon Baptist Convention Health Services, Bamenda, Cameroon 
Received: 16 Jan 2023 - Accepted: 29 Jan 2023 - Published: 21 Mar 2023
Domain: Otolaryngology (ENT)
Keywords: Vallecula, lipoma, dysphagia, case report
©Bonko Neville et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Bonko Neville et al. Lipoma of the vallecula: a rare cause of upper aerodigestive tract obstruction (case report). PAMJ Clinical Medicine. 2023;11:52. [doi: 10.11604/pamj-cm.2023.11.52.38898]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/11/52/full
Case report 
Lipoma of the vallecula: a rare cause of upper aerodigestive tract obstruction (case report)
Lipoma of the vallecula: a rare cause of upper aerodigestive tract obstruction (case report)
Bonko Neville1,2,&, Acha Everistus1,3, Ghislain Feudjio1,4, Brandon Carl Monika5, Chin Virginia1,2, Nantang Marleens1,2, Nyoma Nancy1,2
&Corresponding author
Lipoma of the vallecula is extremely rare, with fewer than 10 cases reported in literature so far. We present a case of an 81-year-old male with a history of slowly progressing dysphagia, change in voice, and difficulty breathing. Examination of the oropharynx revealed a smooth surfaced, oval mass originating from the base of the tongue and occupying the whole oropharyngeal opening. Computed Tomography (CT) scanning of the neck revealed a mass with features of a lipoma originating from the left vallecula. A diagnosis of left vallecula lipoma was established. Complete excision by transoral open surgical approach was preferred, preceded by tracheostomy. There were no signs of recurrence at 6 months follow-up. Although rare, lipoma should be considered as a differential diagnosis of vallecular masses. Proper assessment of size and adequate preparation of the surgical team is paramount, as large vallecular lipomas may make orotracheal intubation difficult, necessitating tracheostomy tube insertion prior to surgical excision.
Lipomas are benign neoplasms arising from fat tissue and are among the commonest mesenchymal tumors in humans. Lipomas most commonly occur in the subcutaneous tissue and rarely in internal organs. Oropharyngeal, hypopharyngeal and oral cavity lipomas are extremely rare, constituting only about 1 to 4.4% of all benign tumors occurring in these regions [1-3]. Lipoma of the vallecula is extremely rare, with fewer than 10 cases reported in literature so far. Typically, lipomas do not cause significant morbidity, however, oropharyngeal subtypes may present with significant upper aerodigestive tract compromise and may be life-threatening in some cases [2]. We present a case of a large lipoma of the left vallecular in an 81-year-old male, causing upper aerodigestive obstruction. To the best of our knowledge, this is the 6th case in literature.
Patient information: an 81-year-old male presented to our clinic with a one-year history of slowly progressing dysphagia, change in voice, and a 2-week history of difficulty breathing. Initially he was able to tolerate solid feeds but over the two weeks prior to consultation, he was only able to swallow semi-liquid foods with occasional odynophagia. His voice had increasingly become muffled, and breathing was especially difficult when he laid on his back. He occasionally had nasal blockage and rhinorrhea. He denied any neck swellings.
Timeline: in the past, the patient was diagnosed of benign prostatic hypertrophy in March 2018 for which he was having serial follow-ups. In February 2020 he was involved in a road traffic accident in which he sustained injury to his right leg. He only presented to the hospital 3 days later with infection of the wound. He was admitted for debridement under general anesthesia and was discharged for wound care to be continued on an out-patient basis. In December 2020, he was re-admitted for skin grafting of the wound. In August 2021, had a prostatic specific antigen (PSA) assay which showed a high value of 13 ng/mL. A re-biopsy of the prostate returned results that were confirmatory for prostatic carcinoma, for which he was on treatment and follow-up. There was also positive history of long duration cigarette smoking and alcohol consumption of mixed brews.
Clinical findings: on examination, his vital signs were stable, but there was hot-potato voice. Examination of the oropharynx revealed a smooth surfaced, oval mass originating from the base of the tongue and occupying the whole oropharyngeal opening (red arrows on Figure 1). Neck examination was normal. The flexible endoscope could not proceed beyond the nasopharynx due to the obstruction.
Diagnostic assessment: contrast and non-contrast CT scan of the neck showed a well-defined hypodense (-30HU), non-enhancing mass originating from the left vallecula, extending to the oropharynx and abutting the inferior portion of the nasopharynx. The mass measured 52 mm by 40 mm on the axial plane (Figure 2). There was a distinct plane between the mass, base of tongue and lingual surface of the epiglottis. Blood parameters were all within normal ranges. A diagnosis of left vallecular lipoma was made. Differential diagnoses included liposarcoma and base of tongue malignant mass.
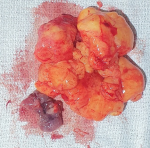
Therapeutic intervention and follow-up: due to difficult intubation, the patient had a tracheostomy done with double barrel 5.0 diameter, cuffed tracheostomy tube. Open excision was done under general anesthesia by transoral route without any complications (Figure 3). The patient resumed oral feeding on post-operative day one. Tracheostomy decannulation was done on post-operative day five following the decannulation protocol, and the patient was discharged home. Histopathology of the excised specimen showed adipose tissue with adipocytes of uniform size, consistent with simple lipoma. Further post-operative recovery after 3 months was uneventful, and the patient was reviewed in 6 months without any evidence of recurrence.
Patient´s perspective: I had so many health challenges, but this is the one I thought would take my life. I saw myself wasting away as the difficulty in swallowing kept getting worse. It was even scarier knowing the problem was in my neck and that blockage of my airway could happen anytime. I am extremely happy the surgery was successful, and now I have no problems at all eating and breathing. Though I still have other health issues to battle with, I remain hopeful.
Informed consent: written consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review.
Lipomas are slow-growing, benign fatty tumours which form soft, lobulated masses enclosed by a thin, fibrous capsule. Lipomas affects about 1% of the population, and more than 90% of these occur in the subcutaneous tissue [4]. About 15 to 20% of lipomas occur in the head and neck region and about 1 to 4.4% of benign tumors in the oral cavity, oropharynx and hypopharynx are lipomas. Though congenital variants exist, lipomas are frequently found in ages over 30 years and prevalence increases with age. Peak age group for occurrence of lipomas is between the 4th and 5th decades of life, and females are more affected than males [1]. The etiology of lipomas is debatable. The trauma theory postulates that micro abrasions leads to fat herniation and subsequent cellular proliferation [5]. Cytokines released from trauma induced inflammation have also been linked to adipocyte differentiation and maturation. In our case, history of long-term cigarette smoking might have engendered some mucosal injury [6], consequently, predisposing to lipoma formation. Associations with gene rearrangements on chromosome 12 have also been identified in cases of solitary lipomas with HMGA2-LPP fusion gene most affected [7]. Though lipomas are benign and asymptomatic in a majority of cases, they could present with life-threatening symptoms, especially when they occur in the upper aerodigestive tract due to obstruction [8]. In the present case, symptoms were slowly progressive over a two-year period and the presence of hot potato voice and occasional nasal obstruction indicates the presence of severe upper aerodigestive obstruction. Detailed history and physical examination are vital in the diagnostic approach to vallecular lipomas. However, patients will likely present to hospital when obstruction has already fully set in. Imaging modalities include Computed Tomography (CT) scanning, which can definitively diagnose a lipoma in virtually all cases owing to its characteristic feature of homogeneous low attenuation that measures between -65 and -125 Hounsfield Units (HU) [9].
Lipomas usually have very thin capsules which can be easily separated from adjacent tissues. Magnetic Resonance Imaging (MRI) shows better soft tissue differentiation and thus shows more details, but is however not readily accessible in terms of cost and time. The present case showed typical features of lipoma arising from the left vallecula. Histologically, lipomas can be classified as either simple lipomas or their variants, which include spindle cell lipomas, fibrolipomas, intramuscular lipomas, angiolipomas, myxolipomas, salivary gland lipomas, pleomorphic lipomas and atypical lipomas [10]. Over 80% are simple lipomas. In the present case, histological sections revealed adipose tissue with adipocytes of uniform size, consistent with simple lipomas. There was no significant nuclear atypia, no lipoblasts, mitosis, or necrosis identified, confirming its benign nature. Differential diagnoses of vallecular masses include mucous retention cysts, which are generally small and are mostly detected incidentally and remain asymptomatic. However, predominantly large vallecular masses, though rare, may include large ductal cysts, dermoid or epidermoid cysts, and some malignant masses originating from the tongue base or supraglottis and extending to the vallecula. Surgical treatment is the best approach to guarantee non-recurrence. Surgical approaches include open, or endoscopic approaches. Size is the main determinant of surgical approach, as large lipomas may render endoscopic approach tedious and unsuccessful [2]. For our patient, transoral open surgical approach was preferred, preceded by tracheostomy due to large size and difficult orotracheal intubation. Complete removal reduces the risk of recurrence. Prognosis with lipomas is usually excellent. However, long-term follow-up is needed owing to the possibility of initial missed diagnosis of liposarcoma as histological differentiation of lipoma and low-grade liposarcoma can be difficult [2].
Although rare, lipoma should be considered as a differential diagnosis of vallecular masses. Proper assessment of size and adequate preparation of the surgical team is paramount, as large vallecular lipomas may make orotracheal intubation difficult, necessitating tracheostomy tube insertion prior to surgical excision.
The authors declare no competing interests.
Bonko Neville: patient care, planning, design and writing of the case report. Ghislain Feudjio and Acha Everistus: patient care, planning and revising of the case report. Brandon Carl Monika, Chin Virginia, Nyoma Nancy, and Nantang Marleens: patient care, review and editing of the drafts. All authors were involved in the final approval for submission, including agreement to accountability for the work. All the authors have read and agreed to the final manuscript.
Figure 1: oropharyngeal mass on physical examination
Figure 2: computed tomography (CT) scan showing vallecular mass
Figure 3: excised lipoma specimen with capsule
- Jeyaraj P, Sehgal S. Lipomas of the oral cavity: Importance of meticulous clinical evaluation, imaging and histopathological examination for precise treatment planning. Dent Oral Craniofac Res. 2017;3(6):2-6. Google Scholar
- Mitchell JE, Thorne SJ, Hern JD. Acute stridor caused by a previously asymptomatic large oropharyngeal spindle cell lipoma. Auris Nasus Larynx. 2007 Dec;34(4):549-52. PubMed | Google Scholar
- Sy A, Nao EEM, Ndiaye M, Taddio JM, Pegbessou EP, Ndiaye C. Lipoma of the soft palate: a rare anatomoclinical entity. PubMed. 2010;127(4):191-193. PubMed | Google Scholar
- Gaskin CM, Helms CA. Lipomas, Lipoma Variants, and Well-Differentiated Liposarcomas (Atypical Lipomas): Results of MRI Evaluations of 126 Consecutive Fatty Masses. Am J Roentgenol. 2004 Mar;182(3):733-9. PubMed | Google Scholar
- Copcu E, Sivrioglu NS. Posttraumatic lipoma: analysis of 10 cases and explanation of possible mechanisms. Dermatol Surg. 2003 Mar;29(3):215-20. PubMed | Google Scholar
- Onur Ozturka, Izzet Fidancib, Mustafa Unal. Effects of smoking on oral cavity. J Exp Clin Med. 2017;34(1):3-7. Google Scholar
- Kubo T, Matsui Y, Naka N, Araki N, Goto T, Yukata K et al. Expression of HMGA2-LPP and LPP-HMGA2 fusion genes in lipoma: identification of a novel type of LPP-HMGA2 transcript in four cases. Anticancer Res. 2009 Jun;29(6):2357-60. PubMed | Google Scholar
- Jessica Lunn, Rajeev Mathew , Prince Modayil. Oropharyngeal lipoma; a rare and dangerous cause of voice change. BMJ Case Rep. 2019 Aug 1;12(7):e230161. PubMed | Google Scholar
- Kransdorf MJ, Bancroft LW, Peterson JJ, Murphey MD, Foster WC, Temple HT. Imaging of fatty tumors: distinction of lipoma and well-differentiated liposarcoma. Radiology. 2002 Jul;224(1):99-104. PubMed | Google Scholar
- Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA. Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 cases. Int J Oral Maxillofac Surg. 2003 Feb;32(1):49-53. PubMed | Google Scholar