Presacral neurilemmoma with fecal incontinence, mimicking mature ovarian teratoma: a case report
Seon Mi Lee, Jae Yoon Jo, Sunmin Kim
Corresponding author: Seon Mi Lee, Department of Obstetrics and Gynecology, Gyeongsang National University Changwon Hospital, School of Medicine, Changwon, Korea 
Received: 14 Mar 2020 - Accepted: 04 Apr 2022 - Published: 06 Apr 2022
Domain: Gynecology
Keywords: Presacral neurilemmoma, pelvic neurilemmoma, presacral schwannoma, pelvic schwannoma, pelvic teratoma, case report
©Seon Mi Lee et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Seon Mi Lee et al. Presacral neurilemmoma with fecal incontinence, mimicking mature ovarian teratoma: a case report. PAMJ Clinical Medicine. 2022;8:52. [doi: 10.11604/pamj-cm.2022.8.52.22338]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/8/52/full
Case report 
Presacral neurilemmoma with fecal incontinence, mimicking mature ovarian teratoma: a case report
Presacral neurilemmoma with fecal incontinence, mimicking mature ovarian teratoma: a case report
Seon Mi Lee1,&, Jae Yoon Jo2, Sunmin Kim3
&Corresponding author
It is very rare that uncommon presacral neurilemmoma is observed along with a teratoma in the ilpsilateral ovary. We report a case of a 66-year-old woman. She presented with fecal incontinence that had lasted 2 months; physical examination revealed no abnormalities. Imaging test results of the pelvis revealed cystic masses suspected of being mature teratomas in the left presacral area and left ovary. Laparoscopic left salpingo-oophorectomy and presacral mass excision were performed; the final pathological diagnosis was neurilemmoma in the presacral area and mature teratoma in the left ovary. Fecal incontinence resolved following surgery, and no adverse events were observed during or after the patient´s hospitalization. Benign neurilemmoma is noninvasive and must be differentiated histopathologically from another invasive peripheral nerve sheath tumor. Also, because neurilemomma observed in the presacral area can be confused with other gynecologic diseases, it is necessary for gynecologists to be aware of it.
Neurilemmoma, also known as schwannoma, is a tumor of the peripheral nerve sheath. Neurofibromas with invasive characteristics are also nerve sheath tumors, and so for diagnostic purposes, the two must be differentiated histopathologically [1]. Neurilemmomas are noninvasive and benign, and they occur predominantly in the head and neck or in the extremities [2]; they rarely occur in the pelvic space or retroperitoneal area [2]. Therefore, neurilemmomas occurring in the pelvic space in women are easily confused with gynecological diseases, such as uterine fibroids, ovarian teratomas, inflammatory abscesses, and malignant ovarian tumors. Cases involving such confusion have been reported [3-6]. Although neurilemmomas are usually asymptomatic and discovered incidentally, those occurring in the pelvis can cause symptoms through mass effects as a result of their location and size. In most of the reported cases, symptoms have included abdominal distension, palpable mass, and constipation as a result of the huge mass size [2,3,5]. However, fecal incontinence is rarely caused by compression of the presacral nerve by the mass. Furthermore, a neurilemmoma tends to be observed more often in men (aged 20-50 years) than in women. We report a rare case of neurilemmoma observed in the presacral area and causing fecal incontinence in a 66-year-old woman.
Patient information: a 66-year-old woman presented with fecal incontinence that had lasted 2 weeks. Although a previous medical checkup had revealed a pelvic mass, she did not seek treatment because she had no uncomfortable symptoms. Her past medical history included no other diseases, and blood tests revealed no specific abnormalities.
Clinical findings: physical examination revealed no abdominal tenderness, and no mass was palpable. Gynecological examination yielded no specific findings.
Diagnostic assessment: transvaginal ultrasonography revealed a heterogeneous echoic mass in the left ovary and a heterogeneous echoic mass in the left pelvic cavity. Pelvic computed tomography revealed a mass of mixed fat and calcified components in the left ovary and a presacral mass of heterogeneous density, which was suspected of being a teratoma. Magnetic resonance imaging (MRI) was additionally performed to determine the presence of sacral nerve damage and spinal cord abnormalities that might explain the fecal incontinence. MRI indicated that the left presacral mass extended to the sacral foramen had low to intermediate signal intensity on T1-weighted images and had high signal intensity on T2-weighted images (Figure 1 A,B,C). In accordance with the imaging results, we thought the two masses were teratomas in the left ovary and left presacral area.
Therapeutic intervention: we performed laparoscopic left salpingo-oophorectomy with presacral mass excision to remove the two masses. The presacral mass was ovoid, measuring 3.0 × 4.0 cm, and the left ovarian mass was oval, measuring 3.0 cm, and both were histologically examined. The histological examination revealed that the presacral mass appeared as a well-defined spindle cell tumor with a prominent cellular component (Antoni A pattern), along with an area of vacuolar changes in the cytoplasm and loss of cellular cohesion (Antoni B pattern) (Figure 2 A). Immunohistochemical study revealed positivity for S100 protein (Figure 2 B). Histological examination of the left ovarian mass revealed a prominent gastrointestinal tract component with proper muscle layer and focal portions of the thyroid tissue (Figure 2 C,D). The final pathological diagnoses were neurilemmoma (the presacral mass) and mature teratoma (the left ovarian mass).
Follow-up and outcome of interventions: after the operation, the fecal incontinence resolved, and the patient had no specific symptoms during the rest of her hospitalization. The patient was discharged on the ninth day following surgery. In the 2 years since the surgical treatment, the patient has remained in good condition with no complications.
Informed consent: the patient consented to the publication of this case report, including her clinical data, because her case was very rare, and she thought that the report would be helpful in the diagnosis and treatment of similar cases in the future.
First named “neurilemmoma” by Masson, this tumor originates from the Schwann cells of the neural sheath [5]. It can occur in the nerve sheath of any peripheral nerve cell, but it is commonly found in the head, neck, and extremities, and it tends to be found mainly in men in their 20s-50s rather than in women [3]. It is rarely found in the pelvis and retroperitoneal area; neurilemmomas in such locations account for approximately 0.7%-2.7% of cases [6]. Neurilemmomas are usually noninvasive and benign, grow slowly, and are often asymptomatic. However, symptoms may be caused by a mass effect that results from the location and size of the tumor [7]. According to reports of neurilemmoma of the pelvis and retroperitoneal area, manifestations such as constipation, abdominal distension, and palpable masses are usually caused by huge masses [2,3,5]. Cases of fecal incontinence caused by compression of the sacral nerve, however, have rarely been reported. Neurilemmomas of the pelvic cavity and retroperitoneal area with regular margins that manifest as round masses causing nonspecific symptoms may be confused with other gynecological diseases involving other adjacent organs; thus, they are difficult to diagnose before surgery. In our patient, in fact, we originally misdiagnosed the tumor in the presacral area as a teratoma. In some cases, as in ours, a huge neurilemmoma in the presacral area has been misdiagnosed as malignant ovarian tumor [3], preoperatively diagnosed as a teratoma [4], misdiagnosed as a uterine fibroid [5], and in a retroperitoneal location, misdiagnosed as a psoas abscess [6].
Imaging tests such as ultrasonography, computed tomography, and MRI are often used for diagnostic purposes prior to surgical treatment; MRI is more helpful than other imaging tests in confirming neurilemmoma. The characteristic findings of neurilemmoma on MRI are low signal intensity on T1-weighted images and heterogeneous high signal intensity on T2-weighted images [2]. In our patient, the MRI findings in the presacral mass were characteristic of neurilemmoma. Neural sheath tumors also include neurofibromas with an invasive tendency, which must be distinguished histopathologically from benign neurilemmomas [1]. Benign neurilemmomas are histopathologically characterized by two main distinct cellular patterns: Antoni A, which consists of prominent nuclear palisading with formation of Verocay bodies [7], and Antoni B, which, conversely, exhibits degenerative changes, including vacuolar changes in the cytoplasm and loss of cellular cohesion [7]. Immunostaining that reveals positivity for S100 is almost diagnostic of neurilemmoma. On the contrary, because neurofibromas are complexes of Schwann cells, fibroblasts, and pericytes, immunostaining for S100 tends to yield negative or weakly positive results [1,7]. On the basis of histological findings, the coexistence of Antoni A and Antoni B cellular patterns, and immunostaining positivity for S100, our patient´s presacral mass was finally diagnosed as neurilemmoma. The appropriate treatment for neurilemmoma is complete surgical excision [3]. However, according to the reports published so far, even if surgical excision is incomplete, the rate of neurilemmoma recurrence is low (approximately 5%-10%), and metastasis has not been reported [5]. We performed complete surgical resection, and as a result, the patient remains in good condition without any other sequelae.
Neurilemmomas in the presacral area are rare. Moreover, cases in which fecal incontinence is caused by compression of the sacral nerve by the mass are very rare. Neurilemmomas in the presacral area in women, as in our patient, can be confused with other gynecological diseases. Although the tumor is benign, and although the rates of recurrence and metastasis are low, complete surgical excision is recommended. Such tumors need to be correctly diagnosed and treated by gynecologists.
The authors declare no competing interests.
Patient management and data collection: SML and JYJ; manuscript drafting: SML and SK; manuscript revision: SML and SK. All the authors have read and agreed to the publication of the final manuscript.
Figure 1: A) T1-weighted axial view shows signal hypointensity of the presacral mass; B) T2-weighted shows signal hyperintensity of the presacral mass, and T2-weighted sagittal view; C) shows signal hyperintensity of the mass extending to the left sacral foramen; nerve damage around the tumor was not observed
Figure 2: histological finding; A) neurilemmoma is composed of Antoni A pattern, consisting of prominent nuclear palisading with formation of Verocay bodies (arrow), and Antoni B cellular pattern, consisting of degenerative changes, including vacuolar changes in the cytoplasm and loss of cellular cohesion (arrowhead); B) S100 protein positive state and histological results of teratoma found in the ipsilateral ovary; C) the mass had mainly a gastrointestinal tract component, including intestinal gland tissue (bracketed by the red line) and focal thyroid tissue (arrow); D) enlarged view of the focal thyroid tissue
- Gleason T, Le BH, Parthasarathy K, Robinson-Bennett B. Obturator nerve schwannoma as a mimic of ovarian malignancy. Case Reports in Obstetrics and Gynecology. 2017;2017:1-4. PubMed | Google Scholar
- Nakashima T, Tsurumaru D, Nishimuta Y, Miyasaka M, Nishie A, Honda H. A case of pelvic schwannoma presenting prominent eggshell-like calcification. Case Reports in Radiology. 2013;2013:1-4. PubMed | Google Scholar
- Samarakoon L, Weerasekera A, Sanjeewa R, Kollure S. Giant presacral schwannoma presenting with constipation: a case report. J Med Case Reports. 2012;6:285. PubMed | Google Scholar
- Ibraheim M, Ikomi A, Khan F. A pelvic retroperitoneal schwannoma mimicking an ovarian dermoid cyst in pregnancy. Journal of Obstetrics and Gynaecology. 2005;25(6):620-621. PubMed | Google Scholar
- Chen CH, Jeng CJ, Liu WM, Shen J. Retroperitoneal schwannoma mimicking uterine myoma. Taiwanese Journal of Obstetrics and Gynecology. 2009;48(2):176-177. PubMed | Google Scholar
- Kishi Y, Kajiwara S, Seta S, Kawauchi N, Suzuki T, Sasaki K. Retroperitoneal schwannoma misdiagnosed as a psoas abscess: Report of a Case. Surgery Today. 2002;32(9):849-852. PubMed | Google Scholar
- Rammohan R, Gupta P, Maini L, Gautam VK. Neurilemmoma of median nerve. Journal of Clinical Orthopaedics and Trauma. 2014;5(1):33-37. PubMed | Google Scholar
Search
This article authors
On Pubmed
On Google Scholar
Citation [Download]
Navigate this article
Similar articles in
Key words
Tables and figures
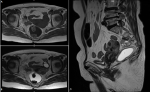 Figure 1: A) T1-weighted axial view shows signal hypointensity of the presacral mass; B) T2-weighted shows signal hyperintensity of the presacral mass, and T2-weighted sagittal view; C) shows signal hyperintensity of the mass extending to the left sacral foramen; nerve damage around the tumor was not observed
Figure 1: A) T1-weighted axial view shows signal hypointensity of the presacral mass; B) T2-weighted shows signal hyperintensity of the presacral mass, and T2-weighted sagittal view; C) shows signal hyperintensity of the mass extending to the left sacral foramen; nerve damage around the tumor was not observed
 Figure 2: histological finding; A) neurilemmoma is composed of Antoni A pattern, consisting of prominent nuclear palisading with formation of Verocay bodies (arrow), and Antoni B cellular pattern, consisting of degenerative changes, including vacuolar changes in the cytoplasm and loss of cellular cohesion (arrowhead); B) S100 protein positive state and histological results of teratoma found in the ipsilateral ovary; C) the mass had mainly a gastrointestinal tract component, including intestinal gland tissue (bracketed by the red line) and focal thyroid tissue (arrow); D) enlarged view of the focal thyroid tissue
Figure 2: histological finding; A) neurilemmoma is composed of Antoni A pattern, consisting of prominent nuclear palisading with formation of Verocay bodies (arrow), and Antoni B cellular pattern, consisting of degenerative changes, including vacuolar changes in the cytoplasm and loss of cellular cohesion (arrowhead); B) S100 protein positive state and histological results of teratoma found in the ipsilateral ovary; C) the mass had mainly a gastrointestinal tract component, including intestinal gland tissue (bracketed by the red line) and focal thyroid tissue (arrow); D) enlarged view of the focal thyroid tissue