Primary hydatid cyst of the thigh: about four cases
Abdelhafid El Marfi, Mohamed Lahsika, Said Senhaji, Hachem Chafik, Ali Krite, Mohamed El Idrissi, Abdelhalim El Ibrahimi, Abdelmajid El Mrini
Corresponding author: Abdelhafid El Marfi, Department of Traumatology Orthopedy B4, University Hospital Hassan II, Fez, Morocco 
Received: 13 Oct 2019 - Accepted: 06 Nov 2019 - Published: 14 Nov 2019
Domain: Infectious diseases epidemiology,Neglected diseases,Orthopedic surgery
Keywords: Hydatid, primary, muscular, thigh, pericystectomy
©Abdelhafid El Marfi et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Abdelhafid El Marfi et al. Primary hydatid cyst of the thigh: about four cases. PAMJ Clinical Medicine. 2019;1:12. [doi: 10.11604/pamj-cm.2019.1.12.20649]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/1/12/full
Primary hydatid cyst of the thigh: about four cases
Abdelhafid El Marfi1,&, Mohamed Lahsika1, Said Senhaji1, Hachem Chafik1, Ali Krite1, Mohamed El Idrissi1, Abdelhalim El Ibrahimi1, Abdelmajid El Mrini1
1Department of Traumatology Orthopedy B4, University Hospital Hassan II, Fez, Morocco
&Corresponding author
Abdelhafid El Marfi, Department of Traumatology Orthopedy B4, University Hospital
Hassan II, Fez, Morocco
The hydatid echinococcosis is preferentially localized in the liver. Muscle localization is very rare, representing less than 1% of the locations of human hydatid echinococcosis. The clinical symptomatology is insidious and not very suggestive, causing a frequent diagnostic delay. the diagnosis is confirmed by imaging: ultrasonography and/or magnetic resonance imaging. The curative treatment remains however surgical. We report a retrospective study over a period of 3 years including 4 cases of primary hydatid cysts of the thigh at the Service of Traumatology-Orthopedics B4 of Hassan II CHU all treated surgically.
The hydatid cyst or hydatidosis is an anthropozoonosis due to the larval form development in humans of tenia (Echinococcosis granulose). It is endemic and constitutes a real public health problem in Morocco. The preferred locations for human echinococcosis are the liver which account for 60% of cases. Other sites of development are the lung (20%), and less frequently the spleen, heart, kidney, central nervous system, bone, and soft tissue [1,2]. The muscular involvement of hydatidosis is an uncommon event, representing less than 1% of human echinococcosis localizations [3,4] because the presence of lactic acid is an unfavorable environment for its growth. The clinical symptomatology is insidious and not very suggestive, causing a frequent diagnosis delay. The hydatidosis muscular can have several imagery aspects that must be known to make the diagnosis preoperatively and prevent the appearance of many serious complications which can be at the origin of diagnostic problem in particular in the absence of pathognomonic radiological signs. The objective of this research article is to point out that, regardless of the site involved, this zoonotic infection should always be considered in the differential diagnosis of any cystic lesion especially in endemic areas.
This is a retrospective descriptive study spread over a period of 3 years (from June 2015 to June 2018) performed at the Department of Traumatology-Orthopedics B4 of CHU Hassan II of Fez and including 4 cases of primary hydatid cysts of the thigh diagnosed and treated all surgically in our service and we have excluded all cases whose the localization was secondary or in another muscular locations on the rest of the human body. We have identified all the epidemiological, clinical and radiological data that have been analyzed to better detail the characteristics of these localization. All our patients were operated using the same operative technique consisting on a pericystectomy in one bloc and they were evaluated at 3 weeks in postoperative, then at 6 weeks after results of histopathological examination.
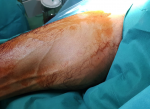
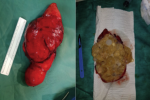
The mean age of our patients was 43 years (range 37 to 55 years) with a sex ratio of 0.33 (1M/3F). All patients who lived in rural areas where raising sheep and contact with dogs was common. Patients consulted for a tumefaction of the soft tissue evolving over more than 3 years which increased in volume progressively (Figure 1). The muscle focus was usually unique and primary. The proximal muscles of the limbs were mainly involved. Ultrasonography was performed for all our four patients and suggested the diagnosis in all cases. The typical characteristic was a liquid echostructure in an endemic context. Magnetic resonance imaging was performed in three of our four patients whose location was deeper (Figure 2). All patients underwent abdominal ultrasound and chest x-ray for other locations and returned negatively. Surgical treatment was used in all cases consisting on a pericystectomy in one bloc (Figure 3) under general anesthesia. It allows us to carry the entire cyst without breaking the wall. In macroscopic aspect, the cystic lesions contents were yellowish, bound and multivesicular (Figure 4). All the parts were sent to the laboratories for histological confirmation. The immediate postoperative course was favorable and no complication was observed. Histopathological examination of the specimen revealed hydatid cyst and showed an inflammatory tissue reaction surrounding "parasite-like cyst". Scoleces were also detected within the surgical specimen. After surgery, all our patients were treated with an additional 1-month course of Albendazole. The resumption of walk was started the day after the operation and there was no problem observed. At the last follow-up (18 months), clinical, biological and ultrasound surveillance did not indicate local or distant recurrence.
Echinococciasis or hydatid disease is a cosmopolite antropozoonosis common to humans and several mammal species. The disease results from the development of the larval or hydatid form of canine tenia (Echinococcus granulosis) in the organism. Hydatid cysts are rarely found in muscles even in endemic areas. Its frequency varies from 1 to 5% [3,5]. Hexacanth embryos that enter the digestive tract are most often stopped by the filters that make up the liver and lungs. A very small quantity arrives even in the great circulation where they disseminate throughout the body. The rarity of muscle sites is explained by the fact that continual muscular contractions and lactic acid production impede the implantation of scoleces [5-7]. Several factors could explain the exceptional nature of the muscular localizations of hydatid cysts: efficacy of the hepatic and pulmonary barriers, muscular environment unfavorable to the growth of hydatid larvae [8]. A lot of muscles localizations have been described, the involvement predominates in the muscles of the neck, trunk and root of the limbs [3,9,10]. The predominant localization in the proximal muscles of the lower limbs could be explained by the volume of the muscle mass and the richness of its blood supply [8]. The incubation period can last from five to 20 years and symptoms occur several years after exposure [11]. The clinical symptomatology is insidious and not very suggestive, causing a frequent diagnostic delay. The clinical presentation, which is not very specific, can be summed up as a non-inflammatory, painless tumefaction gradually increasing in volume over the years, with preservation of the general state [3,10].
However, a number of cysts are revealed by complications such as nerve compression or infections simulating a hot abscess or a malignant tumor [5,12]. Imaging tools such as ultrasound and computed tomography (CT) reveal a calcified cystic wall and microcalcifications within daughter cysts with a fluid density between the cyst and surrounding organs [13]. Magnetic resonance imaging (MRI) interpretation of hepatic KH is well known, but diagnosis is more difficult in soft tissue because imaging interpretations are not well described [4,13,14]. It allows, thanks to its high resolution in contrast, to better study the locoregional extension of the lesion and its relationship with the vasculonervous pedicles, while offering a careful analysis of the cystic walls [5,6,12]. Various serological tests can help in the diagnosis of echinococcosis. However, serology alone is not sufficient for diagnosis. The sensitivity and specificity of serological tests are not known in patients with hydatid diseases. This serology may be useful for monitoring treatment when it is positive [15]. It is important to establish the diagnosis preoperatively to reduce the risk of anaphylactic shock or dissemination in case of puncture or accidental opening of the cyst during resection. Surgery is required for treatment, ideally by total pericystectomy on one bloc. It allows to carry the entire cyst without breaking the wall. Intraoperative precautionary measures using fields soaked with hypertonic saline on the margins of the operative wound help to prevent local dissemination of scoleces [16,17]. However, exeresis of hydatid cysts from the soft tissues is sometimes problematic: the usual absence of cleavage planes, especially when the cyst is infected and adhesions to the vasculonervous elements that can be particularly tight, makes it difficult to perform a complete resection [5]. Recent years have been marked by the development of percutaneous interventional radiology such as puncture-aspiration-injection and re-aspiration (PAIR), and percutaneous drainage without reaspiration, which has improved the hydatid cyst mortality and morbidity. Medical treatment with imidazoles has little efficacy for the treatment of muscular hydatid disease. However it is indicated in inoperable cases or in addition to surgery when the cyst has complicated rupture [16].
The hydatid cyst of the soft tissues remains a rare entity, with progressive development. This diagnosis should be considered, especially in subjects from a high-endemic zones. MRI is the most useful imaging tool for hydatid pathology of the soft tissues whenever ultrasound and CT are insufficient to characterize the hydatid cyst and to determine its relationship to vascular and nerve neighborhood structures. Radical perkystectomy without rupture of the cyst is the treatment of choice but the best way to fight against hydatid disease, whatever its localization, is the prevention. The limits of our study were the reduced number of our population sample and the other muscular locations on the rest of the human body.
What is known about this topic
- The hydatidosis is endemic and constitutes a real public health problem;
- The preferred locations for human echinococcosis are the liver.
What this study adds
- To think of the hydatid cyst in the differential diagnosis of any cystic lesion occurring in a subject living in an endemic area;
- The importance of radical treatment by perikystectomy in a one bloc for better results and especially to avoid recurrences.
The author declare no competing interests.
All the authors have read and agreed to the final manuscript.
Figure 1: hydatid cyst of the adductor compartment: pre-operative aspects
Figure 2: MR Image
of adductor compartment's hydatid cyst
Figure 3: pericystectomy in one bloc
Figure 4: macroscopic aspect of the excised mass
- Kourias B. À propos de 2000 cas de kystes hydatiques opérés. Presse Méd. 1961;69:165-168.
- Ferrandez HD, Gomez-Castresana F, Lopez-Duran L, Mata P, Brandau D, Sanchez-Barba A. Osseous hydatidosis. J Bone Joint Surg Am. 1978 Jul;60(5):685-90. PubMed | Google Scholar
- Akjouj S, El Kettani N, Raissouni Z, Semlali S, Aziz N, Amil T et al. Quel est votre diagnostic. Journal de Radiologie. 2006; Jul 1:87(7-8):989-91. Google Scholar
- Guthrie JA, Lawton JO, Chalmers AG. Case report: the MR appearances of primary intramuscular hydatid disease. Clin Radiol. 1996 May;51(5):377-9. PubMed | Google Scholar
- Cissé AM, Nassar I, Hammani L, Dafiri R, Imani F. Primary extensive hydatidosis of the thigh: unusual radiological aspects. J Radiol. 2002 Nov;83(11):1778-80. PubMed | Google Scholar
- Durakbasa MO, Kose O, Islam NC, Kilicoglu G. A primary hydatid cyst of the gracilis: a case report. J Orthop Surg. 2007 Apr;15(1):118-20. PubMed | Google Scholar
- Kazakos CJ, Galanis VG, Verettas DA, Polychronidis A, Simopoulos C. Primary hydatid disease in femoral muscles. J Int Med Res. 2005 Nov-Dec;33(6):703-6. PubMed | Google Scholar
- Kehila M, Allegue M, Abdessalem M, Letaief R, Said R, Khalfallah A et al. Hydatid cyst of the psoas muscle. Apropos of a case. 1987;68(4):265-8. PubMed
- Combalia A, Sastre-Solsona S. Hydatid cyst of gluteus muscle: two cases, Review of the literature. Joint Bone Spine. 2005 Oct;72(5):430-2. PubMed | Google Scholar
- Meddeb N, Bachrouch N, Elleuch M, Sahli H, Cheour E, Labib S et al. Hydatid cyst of the adductor muscles. MRI aspect, Apropos of 1 case. 2001 May;94(2):106-8. PubMed | Google Scholar
- Amar MF, Chbani B, Lahrach K. Kyste hydatique primitif de la cuisse révélé par une cruralgie. À propos d'un cas. Journal de Traumatologie du Sport. 2010;27:146-148. Google Scholar
- Hammami T, Noomane F, Ketata M, Ganneme Y, Nasr M, Zouari K et al. Hydatid cyst of the thigh: three cases. Rev Chir Orthop Reparatrice Appar Mot. 2002 Apr;88(2):193-6. PubMed
- Garcia-Diez AI, Ros Mendoza LH, Villacampa VM, Cozar M, Fuertes MI. MRI evaluation of soft tissue hydatid disease. Eur Radiol. 2000;10(3):462-6. PubMed | Google Scholar
- Rask MR, Lattig GJ. Primary intramuscular hydatidosis of the sartorius: Report of a case. J Bone Joint Surg. 1970 Apr;52(3):582-4. PubMed | Google Scholar
- Bonitacino A, Carino R, Caratozzolo M. L'échographie dans l'hydatidose. Symposium international sur l'hydatidologie. Med Chir Dig. 1989;18:301-12.
- Daoudi A, Loudiyi WD, Elibrahimi A, Elmrini A, Chakour K, Boutayeb F. Le kyste hydatique sous-cutané solitaire de la région glutéale: une localisation inhabituelle; a propos d'un cas. Ann Chir Plast Esthet. 2008;53:448-51. Google Scholar
- Daoudi A, Shimi M, Lahrach K, Elibrahimi A, Loudiyi WD, Amar MF et al. Échinococcose isolée du muscle flexor digitorum profondus: à propos d'un cas. Chir Main. 2009;28:175-9. Google Scholar