Uncommon case of abdominal pregnancy with spontaneous uterine rupture at 35 weeks
Abderrahim Siati, Anas Nah, Imane Benmouna, Abdelaziz Baidada, Aicha Kharbach
Corresponding author: Abderrahim Siati, Gynecology and Obstetrics Department, Maternity Souissi, University Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco 
Received: 12 Nov 2019 - Accepted: 15 Nov 2019 - Published: 19 Nov 2019
Domain: Obstetrics and gynecology,General surgery
Keywords: Abdominal pregnancy, rupture, cesarean scar
©Abderrahim Siati et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Abderrahim Siati et al. Uncommon case of abdominal pregnancy with spontaneous uterine rupture at 35 weeks. PAMJ Clinical Medicine. 2019;1:19. [doi: 10.11604/pamj-cm.2019.1.19.20959]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/1/19/full
Uncommon case of abdominal pregnancy with spontaneous uterine rupture at 35 weeks
Abderrahim Siati1,&, Anas Nah1, Imane Benmouna1, Abdelaziz Baidada1, Aicha Kharbach1
1Gynecology and Obstetrics Department, Maternity Souissi, University Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco
&Corresponding author
Abderrahim Siati, Gynecology and Obstetrics Department, Maternity Souissi, University
Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco
Abdominal pregnancy is a rare form of ectopic pregnancy and is frequently misdiagnosed. Here, we report a case of abdominal pregnancy with spontaneous uterine rupture of the cesarean-section scar at 35 weeks. A 26-year-old Moroccan woman, G2P2, with a previous caesarean section, was presented to the hospital at 35 weeks of pregnancy with the chief complaint of abdominal pain and vaginal bleeding. Ultrasonography identified the term of an abdominal pregnancy without fetal cardiac activity. An abdominal computed tomography was confirmed the diagnosis of abdominal pregnancy with hemoperitoneum. An emergency laparotomy was performed. The dead male fetus was extracted uneventfully. The placenta which was developed through the cesarean-section scar, was attached to intestines and it was removed with great caution and secured haemostasis. The exploration was showed a complete rupture of the cesarean-section scar which was sutured in two layers. The patient was transfused with 2 units of packed red blood cells, and she was discharged from the hospital on the 10th postoperative day. The abdominal pregnancy is an extremely rare diagnosis. The suspicious case of abdominal pregnancy should be referred to the experienced clinicians in the centres with diagnosis facilities.
Abdominal pregnancy is a rare form of ectopic pregnancy with high morbidity and mortality for both the mother and the fetus. Ectopic pregnancy represents about 1-2% of all pregnancies, with 95% of those occurring in the fallopian tubes [1]. The incidence of abdominal pregnancy differs in various publications and ranges between 1:10,000 and 1:30,000 pregnancies [2]. Diagnosis can be frequently missed in most poor-resource settings because of poor antenatal coverage, low socioeconomic status in most of the patients as well as lack of adequate medical resources [3]. Advanced abdominal pregnancy is still rare, and guidelines for its management are yet unclear with few cases published to date in Africa [4]. We present a rare case of abdominal pregnancy with spontaneous uterine rupture of the cesarean scar at 35 weeks.
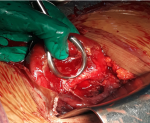
A case of 26-year-old Moroccan woman, G2P2, with a previous caesarean section, was presented to our emergency department at 35 weeks' gestation. The principal complaint on arrival was lower abdominal pain with vaginal bleeding. According to the patient, she was taking regular antenatal care at the rural health centre in her village. The symphysio-fundal height grew steadily up to 28 cm at the last visit, with a presumed cephalic presentation. The patient did not perform any ultrasound during the current pregnancy. On physical examination, she had a heart rate of 102 beats/min, her blood pressure was 109/71mmHg, a respiratory rate of 16 breaths/min and temperature of 37.4°C. Her abdomen was distended, and the fetal parts were palpated under the maternal abdominal wall, with difficulty in specifying the presentation. The sounds of the fetal heart were not perceived. On vaginal examination, the cervix was closed with abnormal bleeding. An ultrasound scanning was done which revealed an abdominal pregnancy without fetal cardiac activity at 35 weeks.The uterus was empty and the placenta appeared to be attached to the fundus. In addition, an abdominal computed tomography was confirmed the diagnosis of abdominal pregnancy and showed hemoperitoneum (Figure 1). An emergency laparotomy with a midline vertical incision was then indicated. At the opening of the peritoneum, a bloody fluid was sucked up. The fetus that bathed in the abdominal cavity was extracted dead and macerated weighing 2400g. The placenta was attached to intestines and it was removed with great caution and secured haemostasis. The exploration was revealed a complete rupture of the cesarean-section scar (Figure 2) which was sutured in two layers. The patient was transfused with 6 units of packed red blood cells intra-and postoperative period. She was kept in the hospital for 10 days postoperatively and discharged home with a follow-up appointment in one month.
Abdominal pregnancy can be classified as primary or secondary. It is primitive in case of direct implantation of the embryo in the abdominal cavity; it is the less common type. It is secondary when it occurs after a ruptured tubal pregnancy or a tubal abortion or even a uterine rupture or perforation [5]. In our case, the abdominal location is secondary because the pregnancy was developed through the incision line of the previous cesarean scare. The clinical expression of abdominal pregnancy is variable, depending on the degree of the anatomical distortion it creates and the placental insertion site [6]. Clinical signs are therefore not specific: abdominal pain with intestinal transit disorder, abdominal pain during active movements of the fetus, spreading of the abdomen due to an irregular presentation, palpation of the fetal parts under the maternal abdominal wall [5,6]. Ultrasound can be very helpful in earlier stages of pregnancy but can be disappointing in later stages. Once the condition is suspected, due to fetal malpresentation, malformations, then purposeful lateral projection sonography and radiography are helpful. An oxytocin stimulation test and the finding of an abnormally high maternal serum alfa-fetoprotein have been proposed [7]. Other radiological studies such as magnetic resonance imaging and computed tomography scan are helpful in the later stages. In our case, we have performed ultrasonography with abdominal computed tomography to confirm the diagnosis. The treatment of abdominal pregnancy is surgical, at best by laparotomy, for a better control of the hemorrhagic risk related to the extraction of the placenta [5,8]. Bleeding from the placental site can be a lifethreatening complication during laparotomy.
It is generally recommended to leave the placenta in situ and monitor the patient's human chorionic gonadotropin levels [2,9]. When the placenta is left in place, it is necessary to keep watch over the appearance of the following maternal complications in post operative period: bowel obstruction, infection, hemorrhage, anemia, fistula [4,10]. These complications can worsen the maternal prognosis, with lethality up to 18% [5,7]. In this case, the placenta was attached to intestines and it was removed uneventfully with great caution. The uterine rupture was sutured in two layers and haemostasis was secured. The case presented here had developed a silent rupture of the incision line linked to the previous cesarean section, through which the abdominal implantation occurred. The fetus continued to grow in the abdominal cavity following a rupture which occurred probably during the first trimester. At 35 weeks of pregnancy, the patient has shown two symptoms of uterine rupture: lower abdominal pain and vaginal bleeding. In the literature, the 12 cases of uterine rupture studied by Teng et al. [11] had a prior history of cesarean section. A silent rupture was identified in four of these 11 patients. For the fetus, it is very important to rule out congenital malformations. There are reports of fetal malformations as high as 40% associated with abdominal pregnancies [2]. When the diagnosis is late, or when it is done intra-operatively, the fetal prognosis is often very pessimistic, with a perinatal mortality which varies between 40% and 95% according to authors [4-6,10]. In this case, it was a dead fetus at 35 weeks' gestation with no congenital malformations.
Abdominal pregnancy, although rare, remains an obstetric emergency that requires attention to diagnosis and management. The pregnant woman must have a good prenatal follow-up. Competent staff in rural health facilities, able to detect the different abnormalities of pregnancy and to indicate adequate treatment is also needed.
The authors declare no competing interests.
All the authors have read and agreed to the final manuscript.
Figure 1: abdominal-pelvic computed tomography shows an abdominal pregnancy
Figure 2: representing complete uterine rupture of the cesarean-section scar
- Isah AY, Ahmed Y, Nwobodo EI, Ekele BA. Abdominal pregnancy with a full term live fetus: case report. Ann Afr Med. 2008 Dec;7(4):198-9. PubMed | Google Scholar
- Baffoe P, Fofie C, Gandau BN. Term abdominal pregnancy with healthy newborn: a case report. Ghana Med J. 2011 Jun;45(2):81-3. PubMed | Google Scholar
- Dabiri T, Marroquin GA, Bendek B, Agamasu E, Mikhail M. Advanced extrauterine pregnancy at 33 weeks with a healthy newborn. Biomed Res Int. 2014;2014:102479. PubMed | Google Scholar
- Sunday-Adeoye I, Twomey D, Egwuatu EV, Okonta PI. A 30-year review of advanced abdominal pregnancy at the mater misericordiae hospital, Afikpo, Southeastern Nigeria (1976-2006). Arch Gynecol Obstet. 2011 Jan;283(1):19-24. PubMed | Google Scholar
- Riethmuller D, Courtois L, Maillet R, Schaal JP. Ectopic pregnancy management: cervical and abdominal pregnancies. J Gynecol Obstet Biol Reprod. 2003;32(7):S101-8. PubMed | Google Scholar
- Worley KC, Hnat MD, Cunningham FG. Advanced extrauterine pregnancy: diagnostic and therapeutic challenges. Am J Obstet Gynecol. 2008 Mar;198(3):297.e1-7. PubMed | Google Scholar
- Masukume G. Live births resulting from advanced abdominal extrauterine pregnancy, a review of cases reported from 2008 to 2013. WebmedCentral Obstet Gynaecol. 2014;5(1):WMC004510. Google Scholar
- Bang Ntamack JA, Ngou Mve Ngou JP, Sima Ole B, Sima Zue S, Mayi Tsonga S, Meye JF. Abdominal pregnancy in Libreville from 1999 to 2009. J Gynecol Obstet Biol Reprod. 2012 Feb;41(1):83-7. PubMed | Google Scholar
- Badria L, Amarin Z, Jaradat A, Zahawi H, Gharaibeh A, Zobia A. Full-term viable abdominal pregnancy: a case report and review. Arch Gynaecol Obstet. 2003;268(4):340-2. PubMed | Google Scholar
- Nassali MN, Benti TM, Bandani-Ntsabele M, Musinguzi E. A case report of an asymptomatic late term abdominal pregnancy with a live birth at 41 weeks of gestation. BMC Res Notes. 2016;9:31. PubMed | Google Scholar
- Teng HC, Kumar G, Ramli NM. A viable secondary intra-abdominal pregnancy resulting from rupture of uterine scar: role of MRI. Br J Radiol. 2007 Jul;80(955):e134-6. PubMed | Google Scholar