Recurrent epigastric pain revealing an aberrant pancreas on endoscopic ultrasonography: a case report
Fatima Belabbes, Nada Faquir, Sara Mounsif, Fedoua Rouibaa
Corresponding author: Fatima Belabbes, Mohammed VI University of Health Sciences (UM6SS), Cheikh Khalifa International University Hospital, Department of Gastroenterology and Proctology, Casablanca, Morocco 
Received: 10 Oct 2022 - Accepted: 12 Nov 2022 - Published: 15 Nov 2022
Domain: Gastroenterology,Intensive care medicine
Keywords: Aberrant, submucosal, endoscopic, ultrasonography, case report
©Fatima Belabbes et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Fatima Belabbes et al. Recurrent epigastric pain revealing an aberrant pancreas on endoscopic ultrasonography: a case report. PAMJ Clinical Medicine. 2022;10:30. [doi: 10.11604/pamj-cm.2022.10.30.37729]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/10/30/full
Case report 
Recurrent epigastric pain revealing an aberrant pancreas on endoscopic ultrasonography: a case report
Recurrent epigastric pain revealing an aberrant pancreas on endoscopic ultrasonography: a case report
Fatima Belabbes1,&, ![]() Nada Faquir1,
Nada Faquir1, ![]() Sara Mounsif 1, Fedoua Rouibaa1
Sara Mounsif 1, Fedoua Rouibaa1
&Corresponding author
Pancreatic heterotopia or aberrant pancreas is a rare birth defect, usually asymptomatic. Its preoperative diagnosis is difficult; the therapeutic attitude remains debated. The clinical implications and embryological description of these rare abnormalities are discussed. We report a case of gastric aberrant pancreas revealed by recurrent epigastric pain. The patient was 57-year-old and had no specific pathological history. She reported several recurrent epigastric pains and presented epigastric pain at admission. Endoscopic examination was performed showing an umbilicated polypoid lesion at the antrum in the stomach. Endoscopic ultrasonography showed a hypoechoic image in favor of an aberrant pancreas. Therefore, we should be aware that a gastric aberrant pancreas can cause recurrent epigastric pain.
The pancreatic tissue existing in an organ or tissue distinct from the pancreas is referred to as aberrant pancreas (AP) [1]. This aberrant pancreas is defined as pancreatic tissue present outside of the pancreas. It has been estimated that about 70% of heterotopic pancreas are found in the stomach, duodenum and ileum [2]. Most patients are asymptomatic, but some may develop symptoms in case of associated complications such as epigastric pain and acute pancreatitis. The diagnosis and treatment of this relatively rare disease are discussed in a comprehensive literature review. Knowledge of these rare morphological variants becomes extremely important because it can greatly contribute to effective patient management. We report our case of gastric aberrant pancreas revealed by recurrent epigastric pain. Outcome and a literature review of the pathology, prognosis, and treatment will be discussed.
Patient information: we report a case of a 57-year-old female with no specific pathological history. She reported a recurrent epigastric pain. She denied history of hypertension, diabetes, coronary heart disease, and any other chronic disease. She presented an abdominal pain, atypical epigastralgia associated with vomiting and constipation evolving for the last 12 years. She didn´t have any weight loss or anorexia.
Clinical findings: general examination found a conscious, apyretic patient that was hemodynamically and respiratory stable, normo-colored conjunctiva, without signs of dehydration. The abdominal exam and the rest of the clinical examination were normal.
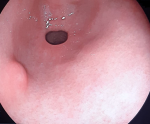
Diagnostic assessment: the results of the laboratory investigations were normal. Lipasemia and liver function tests were normal. The esophagogastroduodenoscopy showed a submucosal lesion of the antrum, umbilicated in the center, with a normal mucosa (Figure 1). The colonoscopy was normal. Biopsies were realized. The histopathology examination did not reveal any abnormalities. The digestive endoscopic ultrasound showed a strictly mucosal lesion, hyperechoic, oval, measuring 8.5 mm long axis, with ductal structure. The muscle layer was preserved (Figure 2).
Diagnosis: this endoscopic ultrasound aspect was in favor of an aberrant pancreas in the gastric wall.
Therapeutic interventions: the patient was hospitalized to complete investigations. She was placed on nil-per-os with parenteral nutrition, rehydration, high-dose proton pump inhibitors (PPI), and analgesic.
Follow-up and outcome of interventions: the patient showed good clinical improvement after regular clinical and endoscopic monitoring.
Patient perspective: during hospital stay and at discharge, the patient's mother was very satisfied with the care.
Informed consent: informed consent was obtained from the patient for us to use the case.
Ectopic pancreas (or aberrant or pancreatic heterotopia) is defined by the presence of pancreatic tissue in an abnormal situation, unrelated anatomically to the main gland [3]. It is an extremely rare pathological condition. The overall frequency of heterotopic pancreas was 0.6 to 13.7% of autopsies and the rate of this lesion in the stomach may be much lower than that [1]. Hunt and bonesteel attributed the first description of this condition to Jean Schultz in 1727, who described it as being present in a diverticulum of the ileum [4]. It is a presence of pancreatic tissue without anatomic or vascular continuity with the normally developed pancreas. The most common heterotopic site is the stomach commonly involving antrum and prepyloric region on the greater curvature or posterior wall [5]. There seems to be considerable divergence of opinion with regard to the distribution over the sexes. Heterotopic pancreas is often found incidentally during surgery or endoscopic examination and is clinically silent and benign [5]. When present, symptoms vary depending on the anatomical location and size of the lesion.
The most frequent presentations may be abdominal pain, a feeling of abdominal fullness and tarry stools [6]. Their symptoms are sometimes associated with the presence or course of pancreatic heterotopias, aberrant pancreas which can cause complications including inflammation, ulceration, bleeding, and obstruction. Cancerous degenerations have been reported in adults [7]. The diagnosis is difficult before surgery, even after abdominal (CT) scan [8]. More characteristic features of abdominal computed tomography (CT), and imaging magnetic resonance (MRI) and endoscopic ultrasonography (EUS) have been reported to help differentiate ectopic pancreas from other submucosal tumors [9]. Heterotopic pancreas of the stomach and duodenum has characteristic CT findings that differ from those of gastric submucosal tumors such as gastrointestinal stromal tumor (GIST) and leiomyoma. However, contrast-enhanced computed tomography can sometimes demonstrate non diagnostic findings such as exophytic bowel wall lesions or mural wall thickening [9]. Endoscopically, the usual manifestations of aberrant pancreas in the stomach have been well described. Central umbilication of the gastric mass has often been noted, and has been attributed to an abortive attempt at duct formation by the aberrant tissue [10].
Endoscopic ultrasound fine-needle aspiration (EUS-FNA) is performed to obtain pathological diagnoses from subepithelial lesion, but the accuracies of such diagnoses are not high enough [9]. However, definitive diagnosis is only obtained with histologic assessment. Several therapeutic options have been proposed such as laparoscopic resection, EMR and ESD [11]. It is controversial to treat asymptomatic patients with gastric aberrant pancreas. For symptomatic patients, surgery is indicated to relieve symptoms [1]. In ectopic pancreas, it would seem that limited resection with healthy margins is sufficient; however, no recommendations could be established due to the rarity of such cases.
The limitation of our study is that the patient was not operated.
Heterotopic pancreas tissue is an extremely rare disease. Patients with an aberrant pancreas are usually asymptomatic, they are discovered incidentally during endoscopy, surgery or autopsy. It is a rare variant interesting to know as it is a rare cause of epigastralgia. It should be considered as a differential diagnosis of submucosal tumors. The rarity of this anomaly has encouraged us to share this manuscript.
The authors declare no competing interests.
Patient management and manuscript drafting: Fatima Belabbes. Manuscript revision: Fatima Belabbes, Fedoua Rouibaa, Nada Faquir and Sara Mounsif. Fatima Belabbes performed the endoscopy. All the authors have read and agreed to the final manuscript.
Figure 1: endoscopic image showing an aspect of extrinsic compression umbilicated in the center with mucosa of normal appearance
Figure 2: digestive endoscopic ultrasound showing a strictly mucosal lesion, hyperechoic, oval, measuring 8.5 mm long axis
- Yen-Chun C, Hoy-Hung C, Kwok-Hung L, Tzung-Jiun T. Ping-I H. Gastric Ectopic pancreas manifested as a subepithelial tumour. Three case reports and a overview. J Pancreas. 2016;17(5):529-34.
- Gokhale UA, Nanda A, Pillai R, Al-Layla D. Heterotopic pancreas in the stomach: a case report and a brief review of the literature. JOP. 2010 May 5;11(3):255-7. PubMed | Google Scholar
- Limaïem F. Pancréas ectopique de localisation hépatique. Pan Afr Med J. 2020;36:250. PubMed | Google Scholar
- Kilius A, Samalavicius NE, Danys D, Zaldokas G, Seinin D. Asymptomatic heterotopic pancreas in Meckel´s diverticulum: a case report and review of the literature. J Med Case Rep. 2015 May 9;9:108. PubMed | Google Scholar
- Subasinghe D, Sivaganesh S, Perera N, Samarasekera DN. Gastric fundal heterotopic pancreas mimicking a gastrointestinal stromal tumour (GIST): a case report and a brief review. BMC Res Notes. 2016 Mar 22;9:185. PubMed | Google Scholar
- Park HS, Jang KY, Kim YK, Yu HC, Cho BH, Moon WS. Cystic lesion mimicking intraductal papillary mucinous tumor arising in heterotopic pancreas of the stomach and synchronous intraductal papillary mucinous adenocarcinoma of the pancreas. Int J Surg Pathol. 2008 Jul;16(3):324-8. PubMed | Google Scholar
- Pouessel G, Michaud L, Pierre MH, Guimber D, Sfeir R, Robert Y et al. Diagnostic endoscopique d´une hétérotopie pancréatique de l´estomac et atrésie de l´oesophage: une association fortuite. Arch Pediatr. 2001 Feb 1;8(2):181-185. Google Scholar
- Littner M, Kirsh I. Aberrant pancreatic tissue in the gastric antrum; report of seven cases. Radiology. 1952 Aug;59(2):201-11. PubMed | Google Scholar
- Yasuda M, Hara K, Kurita Y, Tanaka H, Obata M, Kuraoka N et al. A Novel Method of Diagnosing Aberrant Pancreas: Needle-based Confocal Laser Endomicroscopy. Intern Med. 2018 Oct 1;57(19):2827-2831. PubMed | Google Scholar
- Stone DD, Riddervold HO, Keats TE. An unusual case of aberrant pancreas in the stomach. A roentgenographic and gastrophotographic demonstration. Am J Roentgenol Radium Ther Nucl Med. 1971 Sep;113(1):125-8. PubMed | Google Scholar
- Hirasaki S, Tanimizu M, Moriwaki T, Nasu J. Acute pancreatitis occurring in gastric aberrant pancreas treated with surgery and proved by histological examination. Intern Med . 2005 Nov;44(11):1169-73. PubMed | Google Scholar