Clinical and therapeutic aspects of laparoscopic varicocelectomy: a cross-sectional study in Douala, Cameroon
Nwaha Makon Axel Stéphane, Fouda Jean Cedrick, Landry Oriole Mbouché, Essola Basile, Agbor Orock Tanyi, Soppo Edjenguele Thomas Hassler, Fouda Pierre Joseph, Sosso Maurice Aurelien
Corresponding author: Nwaha Makon Axel Stephane, Faculty of Medicine and Biomedical Sciences, University of Yaoundé 1, Yaoundé, Cameroon 
Received: 16 Jun 2022 - Accepted: 07 Aug 2022 - Published: 05 Sep 2022
Domain: Urology
Keywords: Laparoscopy, varicocele, pain, cameroon
©Nwaha Makon Axel Stéphane et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Nwaha Makon Axel Stéphane et al. Clinical and therapeutic aspects of laparoscopic varicocelectomy: a cross-sectional study in Douala, Cameroon. PAMJ Clinical Medicine. 2022;10:4. [doi: 10.11604/pamj-cm.2022.10.4.35928]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/10/4/full
Research 
Clinical and therapeutic aspects of laparoscopic varicocelectomy: a cross-sectional study in Douala, Cameroon
Clinical and therapeutic aspects of laparoscopic varicocelectomy: a cross-sectional study in Douala, Cameroon
Nwaha Makon Axel Stéphane1,&, ![]() Fouda Jean Cedrick1,
Fouda Jean Cedrick1, ![]() Landry Oriole Mbouché1, Essola Basile2,
Landry Oriole Mbouché1, Essola Basile2, ![]() Agbor Orock Tanyi1, Soppo Edjenguele Thomas Hassler2, Fouda Pierre Joseph1, Sosso Maurice Aurelien1
Agbor Orock Tanyi1, Soppo Edjenguele Thomas Hassler2, Fouda Pierre Joseph1, Sosso Maurice Aurelien1
&Corresponding author
Introduction: varicocele is an abnormal tortuosity of the pampiniform venous plexus and internal spermatic veins that drains the testicle. It is a well-recognized cause of decrease in testicular function, affecting approximately 15-20% of all males and 40% of infertile men globally. Principles of varicocele management consist of interrupting internal spermatic venous reflux while preserving the internal spermatic artery and the vas deferens. Treatment can be obtained through spermatic venous embolization or surgical, which could be performed by open or laparoscopic approach. The purpose of this study was to evaluate the clinical and therapeutic aspects of laparoscopic varicocelectomy in the city of Douala.
Methods: we report a descriptive cross-sectional study including a retrospective and prospective component. We reviewed files of patients who underwent laparoscopic varicocelectomy from January 2015 to May 2021. Clinical and diagnostic components of varicocele, indications and therapeutic outcomes were analyzed.
Results: we total of 71 patients were included in our study. The average age of patients was 34.34 years. Scrotal pain was the most represented clinical sign (46.48%). Varicocele was found on the left in 77.46% of patients. Scrotal pain represented 49.3% of the operative indications, and 81.70% of the patients had their spermatic arteries preserved. Vascular injury was the most common intraoperative complication with 5.63%, while peri-incisional pain (7.04%) was the most common post-operative complication.
Conclusion: laparoscopic varicocelectomy is safe and beneficial with favorable outcome. However, there is limited availability of this approach in our setting, mainly due to lack of technical facilities and practitioners able to popularize it.
Varicocele is an abnormal and tortuosity of the pampiniform venous plexus and the internal spermatic veins that drains the testicle. It is a well-recognized cause of decrease testicular function affecting approximately 15-20% of all males globally [1]. It can result in testicular pain and discomfort, atrophy and has an adverse effect on spermatogenesis and infertility [2]. The cause of testicular injury in patients with varicocele is presumed to be linked to increase scrotal pressure, but the pathogenesis remains poorly understood and could be multifactorial [3]. Several urologists have proven recently that varicocele consists of the most frequent treatable etiology of male infertility worldwide and is found in approximately 40% of males presenting for infertility problems [4]. Clinically grading system defines varicocele as grade 0 (subclinical): non-palpable and visualized only by Doppler ultrasound; grade 1: palpable with valsava maneuver; grade 2: palpable but not visible; grade 3: visible. In the absence of surgical indication, observation remains the management option of adolescents with varicocele. The main indications for surgical treatment of varicocele include; bilateral testicular atrophy, pain and abnormal semen analysis. There are different surgical approaches used in the treatment of varicocele including; inguinal, sub inguinal, retroperitoneal or laparoscopic [5]. Generally, despite evolution of several treatment methods of varicocele, laparoscopy remains one of the most frequently used methods of treatment for bilateral varicocele. In Europe, interventional radiology including microembolisation is more frequently used for treatment of varicocele [6]. The exploitation of laparoscopy in the management of varicocele in resource limited settings like ours is not sufficiently exploited. It is based on this background that we report our experience on laparoscopic varicocelectomy. This includes 71 patients treated for varicocele using laparoscopic approach in two urological units in Douala over a period of 6 years.
Study design and participants: we retrospectively reviewed records of 71 patients who had laparoscopic varicocelectomy over the period of 6 years (January 2015 to May 2021) at the urological surgical unit at the Laquantinie hospital. We included all patients who underwent laparoscopic varicocelectomy indicated for symptomatic varicocele. Varicocele was diagnosed using clinical examination of patients, Valsava maneuver and Doppler ultrasound of the testis was done for all patients. Semen analysis was done for patients who complained of infertility. Symptomatic varicocele was defined as patients with varicocele presenting with scrotal pain, testicular atrophy and altered seminal analysis.
Surgical technique: laparoscopic varicocelectomy was realized under general anesthesia and endotracheal intubation in supine position. All the patients were placed in a urinary catheter to avoid bladder lesion. Pneumoperitoneum was achieved using a veress needle. Insufflation using CO2 was realized by direct puncture at the supra-umbilical region in all our patients (Figure 1). We used 3 working port since all our patients benefited from bilateral varicocelectomy. A 10 mm working port was placed at the supra-umbilical region for the introduction of the camera. Two working ports of 5 mm were placed at each iliac fossa for the dissecting forceps (Figure 2). The internal inguinal ring was identified, and the posterior peritoneum was incised 3 cm above the trajectory of the spermatic vessels (Figure 3). Dilated veins were then identified, dissected secured and clipped while carefully preserving the internal spermatic artery (Figure 4, Figure 5).
Statistical analysis: data on demographics, clinical symptoms, ultrasound findings, operative findings and post-surgical outcomes were recorded for each patient. Data collection was achieved using structured questionnaires by consulting patient records, post-surgical reports and by carefully viewing videos of the different operative procedures. Data were analyzed using EPI info 7.0. parametric variables were reported as means and standard deviations and percentages and counts were used to report categorical variables.
Ethical clearance: study was approved by institutional ethics committee.
A total of 71 files of patients were collected.
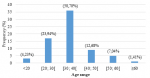
Socio-demographic characteristics: the mean age was 34.34 ± 9.40 years old (range, 16 - 62 years) (Figure 6). Married people were most affected by this pathology, with a frequency of 56.34% compared to singles. Civil servants are the most affected by this pathology at a frequency of 40.85% followed by students in 18.30% of cases.
Clinical features: varicocele was mainly diagnosed in a context of scrotal pain for 33 patients (46.48%) and infertility for 32 patients (45.07%) (Table 1). Other symptoms reported by patients included scrotal discomfort (n = 36.62%), scrotal deformation among 24 (33.8%) and heaviness of scrotum for 18 (25.35%) patients (Table 2). Twelve patients (16.9%) had a history of hypertension and 35 (49.29%) had a past surgical history among which, 8 (22.85%) had previously had a varicocelectomy and 22 (62.85%) had a visceral surgical procedure in the past (Table 3). Our 71 patients had a total of 142 varicocelectomy procedures: 56 (78.87%) cases were unilateral with one case of isolated right varicocele, 15 (21.12%) cases were bilateral and 7(9.86%) patients had recurrent varicocele (Table 4). 41 (57.14%) patients had grade 2 varicocele and only 5 (7.04%) patients had grade 3 varicocele. Scrotal pain was the most reported indication for surgery in our study in 35(49.03%) patients (Table 5).
Operative results: transperitoneal varicocelectomy was performed in all patients, with preservation of spermatic artery in 81.7% of the cases. In all 71 patients, dilated veins were simply clipped without sectioning of spermatic veins. Intraoperative findings included adhesions in 11 (15.49%) patients. Four intraoperative complications were encountered. Vascular injury was encountered in 4(5.63%), and 2 (2.82%) cases were converted to open surgery (Table 6). The vascular injuries were all due to spermatic arterial rupture, and this was the only intraoperative complication encountered. Conversion to open surgery was done in two of these cases, while the other two cases were managed by electrocoagulation of the spermatic artery. These vascular lesions were among patients operated using conservation of spermatic artery technic. The mean duration of hospital stay was 1.51 ± 1.31 days (range, 1 - 7 days). Most patients were discharged on the first day post-surgery.
Outcomes: post-operative evolution was simple in 62 (87.32%) patients. However, we notice surgical site infection in 2 (2.82%) patients despite administration of antibiotic prophylaxis, 5 (7.04%) patients had post-operative pains, 1 (1.41%) patient had hydrocele post-surgery and 1 (1.41%) patient had subcutaneous emphysema at the penis and scrotum (Table 7). The delay period for patients to return to their normal activity was 4.39 ± 4.34 days (range, 2 - 28 days).
A total of 71 patients were included in our study. Our results were lower than those of Yasir SI of Morocco, Abdem SA et al. in Egypt, who had 30 and 18 patients respectively in their studies [7,8]. This could be related to the fact that contrary to Cameroon, laparoscopy is not the only modality in use in treatment of varicocele in these different countries. The mean age of our patients was 34.34 ± 9.40 years. The median age range was 30 and 40 years. This could be explained by the fact that this age group is sexually active and, for desire to procreate, these patients will consult more frequently. Felix Seiler et al. in Germany and Hisham et al. in Emirate found a lower average age of 30.2 and 21.3 respectively [9]. This could be explained by the absence of a system of varicocele screening during medical visits at our different academic institutions. Civil servants (40.85%) and students (18.30%) represented the majority of our participants. Our results are similar to that of Yevi D et al. in Benin, who found civil servants as the most represented profession [8]. This is due to the fact that our study was conducted in an urban setting. 49.29% of patients operated had a past history of surgery among which 62.85% had laparotomy, a reason which could explain the high rate of intraoperative adhesions. Our results are far higher than of Kbaier et al. in Tunisia, who had no past surgical history in their study population [10]. Varicocele was mainly diagnosed in a context of one or more clinical signs of varicocele in 52% of patients and infertility for 32 (45.07%) patients. Yasir S in Morocco reported a lower infertility rate of 23% [11]. Contrary, Kachrilas et al. in England did not report any notion of infertility in their study population. This could be explained by the fact that Caucasian have the attitude of seeking medical consultation earlier compared to our study population who most often auto medicate and consults only when they have a symptomatic health problem and are not habitual to systematic health checks [12]. Among our 71 patients, 77.46% had left varicocele. These results were slightly lower than those of Hisham et al. of the Emirate and Yasir of Morocco and Kachrilas of England who reported left varicocele in 87.93%, 87%, 85.4% respectively among their study participants [9,11,12]. Grade 2 varicocele was the most reported in our study (57.14%), results similar to that reported by Argawal et al. in India with 53.14% of grade 2 varicocele. Contrary, Hassan in the USA had grade 3 varicocele most reported among their participants with a prevalence of 75% [13,14]. Scrotal pain was the most reported indication for surgery in our study (49.03%). This was contrary to the results of Kbaier et al. in Tunisia, who reported infertility as the first indication for surgery among 54.83% of patients [10]. Adhesions were the principal intraoperative findings in 15.49% of our patients. Similarly, Shazly et al. reported 17.8% of intraoperative adhesions among participants. This could be explained by the fact that 30.98% of patients in our study had a past history of visceral surgery [15].
Surgical technic: all our patients were operated using the trans-peritoneal approach and 81.70% of patients had their spermatic artery preserved. This result is lower than that of Kumar et al. and Farag et al. who realized preservation of the spermatic vessels in all their patients [7,16]. This great difference is linked to the fact that our surgical procedures were realized by specialists undergoing Masters training on laparoscopy, who avoid vascular manipulations due to their limited laparoscopic experience. Intra-operative surgical complications occurred in 4 patients (5.63%), essentially vascular lesion, among which two were converted to open surgery and the others were managed using electrocoagulation. This complication rates are higher than those of Shazly et al. and Hassan et al. who did not have any intra-operative complications in their different series [14,15]. This could be explained by the fact that in our study, the surgical procedures were realized by specialized undergoing a masters training in laparoscopy who lack great experience in manipulating laparoscopic equipment. The post-operative complication rate was 12.68%. Several studies have proven the advantage of laparoscopic surgery with respect to reduction of post-operative complications [12,13,17]. Post-surgical evolution was simple in 67 (87.32%) patients, 5(7.04%) patients had post-operative pains. Our results were higher than that of Yasir in Morocco, who did not report any post-operative pain. This difference was linked to the fact that post-operative pains occurred in patients who did not receive analgesics post-surgery [11]. Surgical site infections were reported in 2(2.82%) patients in our series. This result is slightly higher than of Hisham et al. and Akin et al. who had 1case of surgical site infection. This low percentage of surgical site infection could be explained by the fact that all the patients of these different series received preoperative antibiotic prophylaxis [9,17]. Post-operative hydrocele was reported in a single patient (1.41%) and occurred 1 month post-surgery. Johnson in the USA and Abdel et al. reported higher rates of post-operative hydrocele of 17.6% and 10% respectively [5,18]. This difference could be due to the fact that many of our patients did not perform post-operative control testicular ultrasound.
Conversion: during our study, 2(2.82%) patients had conversion to open surgery. This conversion rate is higher than that reported by Abdel et al., Akin et al. and Kachrilas et al. who did not have any case of surgical conversion in their different series [12,17,19]. This difference is probably linked to the fact that the surgeons in our series were less experience with vascular dissections. The mean hospital stay for our patients was 1.51 days, similar to results reported by Shazly et al. in Egypt [15]. However, we noticed a prolonged hospital stay of some patients and this was essentially among patients who had post-operative complications and the patients who had surgical conversion to laparotomy. The mean duration of patients to return to their normal activities was 4.39 days. Yasir et al. reported a shorter mean duration of 2.5 days to return to normal activities among their patients [20]. Our result was due to the fact that many of our patients were scared to their normal activities, given that this surgical approach was new to them.
Laparoscopy is a new technic for varicocele treatment and requires rigorous surgeons training and practice. It is a safe alternative surgical approach for treatment of symptomatic varicocele, and it's becoming feasible in our resource limited settings. It offers the advantage of high rate of symptom regression, less invasive, less post-operative pain, low rate of postoperative hydrocele and reduces time to return to normal activities post-surgery. It is also best indicated in patients with bilateral hydrocele. However, the high-cost due to the limited number of competent surgeons capable of performing this procedure in our setting can´t be neglected.
What is known about this topic
- Laparoscopic varicocelectomy is associated with reduced intra-operative and post-operative complications;
- Laparoscopy is an alternative surgical approach for treatment of symptomatic varicocele.
What this study adds
- Laparoscopic varicocelectomy is new surgical technic in Cameroon;
- Laparoscopic varicocelectomy is a safe alternative surgical approach for treatment of symptomatic varicocele, and it's becoming feasible in our resource limited settings.
The authors declare no competing interests.
Conception and design of study: Nwaha Makon, Mbouche Landry. Acquisition of data: Thomas Hassler, Fouda Jean Cedrick. Analysis and interpretation of data: Essola Basile. Drafting the manuscript: Agbor Tanyi Orock. All the authors have read and agreed to the final manuscript.
Table 1: clinical signs and symptoms presented during consultation
Table 2: circumstance of diagnosis
Table 3: distribution of patients past surgical history
Table 4: topographic distribution of varicocele
Table 5: indications of varicocelectomy
Table 6: intra-operative complications
Table 7: distribution of post-operative outcomes
Figure 1: patient installation in dorsal decubitus position with pneumoperitoneum realized following direct puncture at the supra-umbilical region
Figure 2: introduction of working ports, 10 mm port at the supra-umbilical region and 5mm ports at the right and left iliac fossa
Figure 3: identification of the internal inguinal ring and the trajectory of the spermatic vessels and vas deferens
Figure 4: dissection and isolation of the varicose spermatic veins from the spermatic cord.
Figure 5: double ligation of varicocele using clips
Figure 6: age distribution of study participants
- Wagner L. Varicocèle: physiopathologie et approches thérapeutiques. Androl. 2002;12:100-104. Google Scholar
- Pastuszak. Varicocele and testicular function. Asian J Androl. 2015 Jul-Aug;17(4):659-667. PubMed
- Castagnetti M, Cimador M, Catalano P, DiPace M, Sergio M, De Grazia E. Evolving management of adolescent varicocele. J Pediatr Urol. 2008 Apr;4(2):107-1. PubMed | Google Scholar
- Seiler F, Kneissl P, Hamann C, Jünemann KP, Osmonov D. Laparoscopic varicocelectomy in male infertility: improvement of seminal parameters and effects on spermatogenesis. Wien Klin Wochenschr. 2022 Jan;134(1-2):51-55. PubMed | Google Scholar
- Johnson D, Sandlow J. Treatment of varicoceles: techniques and outcomes. Fertil Steril. 2017 Sep;108(3):378-384. PubMed | Google Scholar
- Emad SAA, Mohammed HE, Ahmed HEHA. Results of laparoscopic varicocelectomy. The Egyptian Journal of Hospital Medicine. 2018;72(1):3823-3826.
- Farag AM, Abo-Elsaad AY, Ahmed YA, Azzam ASM. Laparoscopic varicocelectomy initial experience at Al_Azhar Hospital (Demietta). The Egyptian Journal of Hospital Medicine. 2018;73(11):8077-8083. Google Scholar
- Mohammed M, Kabbash M, Abd Allah H, Saleem A. Laparoscopic versus subinguinal varicocelectomy: comparative study. The Egyptian Journal of Hospital Medicine, 2021;83(1):1597-1601. Google Scholar
- Maghraby HA. Laparoscopic varicocelectomy for painful varicoceles: merits and outcomes. Journal of Endourology. 2002 Mar;16(2):107-10. PubMed | Google Scholar
- Kbaier I, Binous MY, Attyaoui F, Nouira Y, Horchani A. La ligature sous coelioscopie des vaisseaux spermatiques dans le traitement de la varicocèle: à propos de 129 interventions. Ann Urol (Paris). 2002 Oct;36(5):329-33. PubMed | Google Scholar
- Shitu Isa Y. Place de la chirurgie laparoscopique dans le traitement de la varicocèle de l´adulte. Thesis. 2014.
- Kachrilas S, Popov E, Bourdoumis A, Akhter W, El Howairis M, Aghaways I et al. Laparoscopic varicocelectomy in the management of chronic scrotal Pain. JSLS. 2014 Jul-Sep;18(3):e2014.00302. PubMed | Google Scholar
- Agarwal BB, Manish K. Endoscopic varicocelectomy by extraperitoneal route: a novel technique. Int J Surg. 2009 Aug;7(4):377-81. PubMed | Google Scholar
- Hassan JM, Adams MC, Pope JC 4th, Demarco RT, Brock JW 3rd. Hydrocele formation following laparoscopic varicocelectomy. J Urol. 2006 Mar;175(3 Pt 1):1076-9. PubMed | Google Scholar
- El-Shazly M, Eissa B. Laparoscopic varicocelectomy in infertile men: does age matter. Urol Int. 2013;91(2):192-6. PubMed | Google Scholar
- Kumar D, Shiwach DS, Mehra S, Manchanda BV. A prospective study on laparoscopic varicocelectomy: efficacy and safety. IOSR JDMS. 2017;16(3):59-62. Google Scholar
- Akin Y, Ateş M, Yücel S, Başara I, Çelik O, Bozkurt A et al. Comparison of different ligation techniques in laparoscopic varicocelectomy. Turk J Med Sci. 2014;44(2):273-8. PubMed | Google Scholar
- Park SW, Kim TN, Lee W, Park HJ, Lee SD, Park NC. Umbilical laparoendoscopic single site surgery versus inguinal varicocelectomy for bilateral varicocele: a comparative study. Int J Urol. 2011 Mar;18(3):250-4. PubMed | Google Scholar
- Li M, Wang Z, Li H. Laparoendoscopic single-site surgery varicocelectomy versus conventional laparoscopic varicocele ligation: a meta-analysis. J Int Med Res. 2016 Oct;44(5):985-993. PubMed | Google Scholar
- Kattan S. The impact of internal spermatic artery ligation during laparoscopic varicocelectomy on recurrence rate and short post operative outcome. Scand J Urol Nephrol. 2001 Jun;35(3):218-21. PubMed | Google Scholar