Unusual presentation of an invasive mucinous adenocarcinoma (aka-BAC) as cavitating pneumonia: a case report
Lamla Nqwata, Mwakyula Habakkuk Issakwisa, Leodegard Mujwahuzi, David Daniel Nassoro, France Skosana
Corresponding author: Mwakyula Habakkuk Issakwisa, Department of Internal Medicine, Mbeya Zonal Referral Hospital, University of Dar es Salaam Mbeya, College of Health and Allied Sciences (UDSM-MCHAS), Mbeya, Tanzania 
Received: 01 Jul 2022 - Accepted: 03 Jan 2023 - Published: 05 Jan 2023
Domain: Radiology, Infectious disease, Internal medicine
Keywords: Broncho-alveolar carcinoma, mucinous adenocarcinoma, cavitating pneumonia, consolidation, case report
©Lamla Nqwata et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Lamla Nqwata et al. Unusual presentation of an invasive mucinous adenocarcinoma (aka-BAC) as cavitating pneumonia: a case report. PAMJ Clinical Medicine. 2023;11:3. [doi: 10.11604/pamj-cm.2023.11.3.36162]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/11/3/full
Case report 
Unusual presentation of an invasive mucinous adenocarcinoma (aka-BAC) as cavitating pneumonia: a case report
Unusual presentation of an invasive mucinous adenocarcinoma (aka-BAC) as cavitating pneumonia: case report
Lamla Nqwata1, ![]() Mwakyula Habakkuk Issakwisa2,&, Leodegard Mujwahuzi2, David Daniel Nassoro2, Frans Abram Skosana3
Mwakyula Habakkuk Issakwisa2,&, Leodegard Mujwahuzi2, David Daniel Nassoro2, Frans Abram Skosana3
&Corresponding author
Mucinous adenocarcinoma, previously termed Broncho-alveolar carcinoma aka “BAC”, has a typical radiographic presentation that includes a solitary lesion, Consolidation and a diffuse pattern. A 50-year-old female presented with a productive cough, episodic haemoptysis and significant weight loss, with the initial radiographic finding showing an atypical form of cavitating pneumonia mimicking tuberculosis. Chest CT showed a cavitating lesion of the right lower lobe. There was no clinical or radiographic resolution after treatment with antibiotics. An open lung biopsy was performed and was consistent with invasive mucinous adenocarcinoma. Unfortunately, before the introduction of appropriate therapy, respiratory failure led to her demise. To avoid misdiagnosis, clinicians in areas with high TB incidences should be aware of the atypical presentation of mucinous adenocarcinoma as it can mimic infectious processes, as in our case. Early diagnosis avoids delays in initiating proper treatment and resultant poor outcomes.
Bronchoalveolar carcinoma (BAC), now termed pulmonary mucinous adenocarcinoma, is a non-small cell lung cancer (NSCLC) and represents 6.5% of pulmonary neoplasms [1]. This tumour typically presents as a solitary lesion, consolidation and diffuse pattern. The rationale for writing the case stems from the unusual radiological presentation of the BAC, which is not in keeping with typically described patterns, namely solitary lesion, consolidation and diffuse disease [2]. More importantly, cavitating pneumonia in a patient with no risk factors for malignancy in our setting with a high burden of tuberculosis and other necrotising infections will most of the time be treated as an infective process as in this case, leading to delays in diagnosis with resultant devastating outcomes. Lastly, we want to highlight the typical patient profile of the patients with BAC, which does not conform to most lung malignancies, usually in younger females and non-smokers with no apparent risk factors for malignancy [3].
Patient information: a 50-year-old black African female without a background history of smoking was referred from a private health care facility after a one-year history of coughing mucopurulent sputum, episodic haemoptysis and significant weight loss. She accounts for having been treated with several antibiotics and a complete course of antituberculous drugs without any symptomatic improvement.
Clinical findings: her physical examination was significant for tachypnoea, temporal wasting and bilateral crackles.
Timeline of current episode: this patient had attended several hospitals in different settings, she was treated for bacterial pneumonia and later pulmonary tuberculosis without any improvement until she arrived at our pulmonology clinic with worsening symptoms.
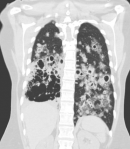
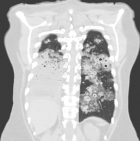
Diagnostic assessment: a chest X-ray (Figure 1) and CT chest (Figure 2) from a peripheral hospital in early 2021 uncovered a cavitating lesion in the medial basal segment of the right lower lobe. A follow-up CT chest (Figure 3) revealed a cavitating lesion with surrounding ground-glass opacities. She arrived at our hospital in early 2022 due to further clinical deterioration. We did a workup for the infective process in conformity with the radiological pattern and the prevalence of diseases in South Africa. Sputum for GeneXpert, TB culture, cytology, and several blood tests that included full blood count, C-reactive protein, kidney function, autoimmune studies were unremarkable. A further CT chest (Figure 4) showed multiple cavitating lesions in both lung fields. An open lung biopsy was consistent with invasive mucinous adenocarcinoma with a negative epithelial growth factor receptor (EGFR). She subsequently progressed to respiratory failure, with a CT chest (Figure 5) showing bilateral cavitating lesions.
Diagnosis: mucinous adenocarcinoma.
Therapeutic interventions: the patient had died before appropriate treatment was instituted.
Patient perspective: maybe it was meant to be.
Informed consent: written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
This case highlights an unusual radiographic presentation of BAC as non-resolving cavitating pneumonia should alert any clinician, even the radiologists [4]. Bronchoalveolar carcinoma (BAC) is a non-small cell lung cancer (NSCLC), accounting for 6.5% of lung malignancies [5]. It is commonly described in younger females between 40 and 70, non-smokers with common cough symptoms, shortness of breath, haemoptysis, and fever [6]. Bronchorrhea is a rare and late manifestation [7]. It has varying radiographic patterns, including solitary lesion, consolidation and a multifocal or diffuse pattern [2]. In our case, the presentation is unusual as it is not of the described radiological patterns of BAC, leading to a delayed diagnosis. One case report by Maskiny et al. described a similar unique presentation of BAC as multifocal bilateral cavitating lesions [8]. The mucinous form of adenocarcinoma is the most aggressive form that responds poorly to treatment [9]. The survival of the majority of patients with lung cancer is poor. The earlier the cancer is diagnosed, the higher the cure rate with surgery. Thus, the starting point of early diagnosis and hence early treatment should be a high index of suspicion in a patient with radiological findings of non-resolving pneumonia. The delay in diagnosis of this rare disease was compounded by fragmented care and poor communication of general practitioners (gatekeepers) who were doing follow-ups for this patient and their seniors.
To avoid missing their diagnosis, gatekeepers and specialists in Africa should be aware of these rare and difficult-to-recognise conditions such as mucinous adenocarcinoma. Missed diagnosis of cancer leads to significant delay in offering adequate treatment. Dare to think rare!
The authors declare no competing interests.
All the authors have read and agreed to the final manuscript.
Figure 1: chest X-ray (2021): right middle zone ill-defined opacity
Figure 2: CT chest (2021): right middle and lower zone cavitating lesion
Figure 3: CT chest (after 3 months of treatment of cavitating pneumonia): right middle and lower zone cavitating lesion with surrounding ground-glass opacity
Figure 4: CT chest (after 1 year of treatment of cavitating pneumonia): bilateral cavitating lesions
Figure 5: CT chest (upon arrival at our facility): extensive dense consolidation of right hemithorax with multiple cavitating lesions on the left hemithorax
- Lee KS, Kim Y, Han J, Ko EJ, Park CK, Primack SL. Bronchoalveolar carcinoma: clinical, histopathologic, and radiologic findings. Radiographics. 1997 Nov-Dec;17(6):1345-57. PubMed | Google Scholar
- Hill CA. Bronchoalveolar carcinoma: a review. Radiology. 1984;150(1):15-20. PubMed | Google Scholar
- Chakraborty RK, Sharma S. Bronchoalveolar Cancer. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2022 Jan. [Updated 2022 Apr 22]. Accessed Jul 01, 2022.
- Patsios D, Roberts HC, Paul NS, Chung T, Herman SJ, Pereira A. Pictorial review of many faces of bronchoalveolar cell carcinoma. Br J Radiol. 2007; 80(960):1015-1023. PubMed | Google Scholar
- Barsky SH, Cameron R, Osann KE, Tomita D, Holmes EC. Rising incidence of bronchioalveolar lung carcinoma and its unique clinicopathologic features. Cancer. 1994 Feb 15;73(4):1163-70. PubMed | Google Scholar
- Ebbert JO, Chhatwani L, Aubry MC, Wampfler J, Stoddard S, Zhang Fang et al. Clinical features of bronchoalveolar carcinoma with new histologic and staging definitions. J Thorac Oncol. 2010 Aug;5(8):1213-20. PubMed | Google Scholar
- Gandhi S, Das B. Bronchorrhea-an uncommon presentation of bronchoalveolar carcinoma. J Assoc Chest Physicians. 2019;7(1):41-44. Google Scholar
- Maskiny CF, Kaleekal T, Rao A, Haasler G. Cavitating bronchoalveolar carcinoma: an unusual radiological presentation. CHEST. 2010;138(4).
- Popat N, Raghavan N, McIvor RA. Severe bronchorrhea in a patient with bronchoalveolar carcinoma. Chest. 2012;141(2):513-514. Google Scholar