Ependymal lined paraventricular neuroglial cyst: an outcome of endoscopic cystoventriculostomy concomitant ventriculoperitoneal shunt procedures (a case report)
Farhad Bal´afif, Tommy Alfandy Nazwar, Donny Wisnu Wardhana, Ulil Abshor, Achmad Bayhaqi Nasir Aslam, Ike Sulistiyowati, Mustofa Mustofa
Corresponding author: Farhad Bal´afif, Division of Neurosurgery, Departement of Surgery, Saiful Anwar Hospital, Malang, Indonesia 
Received: 23 Oct 2022 - Accepted: 18 Feb 2023 - Published: 22 Feb 2023
Domain: Neurosurgery
Keywords: Paraventricular neuroglial cyst, supratentorial lesions, cyst fenestratum concomitant VP-shunt, outcome, case report
©Farhad Bal´afif et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Farhad Bal´afif et al. Ependymal lined paraventricular neuroglial cyst: an outcome of endoscopic cystoventriculostomy concomitant ventriculoperitoneal shunt procedures (a case report). PAMJ Clinical Medicine. 2023;11:44. [doi: 10.11604/pamj-cm.2023.11.44.37925]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/11/44/full
Case report 
Ependymal lined paraventricular neuroglial cyst: an outcome of endoscopic cystoventriculostomy concomitant ventriculoperitoneal shunt procedures (a case report)
Ependymal lined paraventricular neuroglial cyst: an outcome of endoscopic cystoventriculostomy concomitant ventriculoperitoneal shunt procedures (a case report)
![]() Farhad Bal'afif1,&, Tommy Alfandy Nazwar1, Donny Wisnu Wardhana1, Ulil Abshor2,
Farhad Bal'afif1,&, Tommy Alfandy Nazwar1, Donny Wisnu Wardhana1, Ulil Abshor2, ![]() Achmad Bayhaqi Nasir Aslam3, Ike Sulistiyowati3, Mustofa Mustofa1
Achmad Bayhaqi Nasir Aslam3, Ike Sulistiyowati3, Mustofa Mustofa1
&Corresponding author
Neuroglial cysts are one of the problems that might develop in the neuroaxis region. We present the case of a 79-year-old male with an acute decrease in consciousness, dysphagia, and seizure with a past medical history of a cystic mass in the frontal lobe since 5 years ago. A cystic lesion with a calcification component was found in the regio left frontal after the patient received a head CT without contrast. The periventricular white matter is where the lesion is found. Subsequent brain MRI with and without contrast showed hypointense T1 weighted image (T1W1), hyperintense T2-weighted imaging (T2W1), hypointense fluid-attenuated inversion recovery (FLAIR), and non-restricted Diffusion-weighted imaging (DW1). A non-enhancing intra-axial lesion measuring 5.1 cm (AP) x 3.1 cm (LL) x 3.6 cm (CC). Following a discussion of the benefits and risks with his family, the decision was eventually made to proceed with endoscopic cystoventriculotomy (cyst Fenestratum) and concurrent VP-shunting. This method produced positive results. The preferred method is endoscopic fenestration since it carries fewer risks and consequences than open craniotomies and fenestration.
All cysts attached to the ventricular wall are referred to as intraventricular cysts. These include Rathke cleft cysts, colloidcysts, choroid plexus cysts, multiloculated cysts, arachnoid aysts, porencephaly cysts and ependymal cysts. Ependymal cysts are typically neuroepithelial cysts that develop anywhere in the neuraxis from ectopic remnants of primitive neuroglial tissue. However, they are frequently found in the central white matter of the temporal and frontal lobes at the juxtaventricular position [1]. Microscopic examination indicated that the specimen consisted of a thick layer of glial/connective tissue lined by a single layer of cuboidal or columnar epithelium with cilia. In certain areas, papillary structures resembling the choroid plexus were identified as ependymal lined neuroglial or so-called (glioependymal cyst) [2]. No goblet cells were visible in the collection [3]. The location of ependymal cysts in the lateral ventricles is unique. These cysts are thought to develop from embryonic cell inclusions near the neural tube's end, resulting in a mass that resembles the stratum corneum of the epidermis and contains cholesterol crystals [4]. Endoscopic cystoventriculostomy has become typical in recent years. It takes a secure and suitable approach to cope with headaches after treating instances of an ependymal cyst. The preferred sites of formation of intracranial ependymal cysts are the cerebellopontine angle and perimesencephalic cisterns [4]. Intraventricular cysts are commonly treated with open surgery for instance peritoneal shunting, microfenestration with partial excision, endoscopic fenestration, stereotactic aspiration, cystocisternostomy, and cystoventriculostomy [5].
Complications after ependymal cyst removal could indeed happen rather often. These include permanent and transient cranial nerve deficits, hydrocephalus, and aseptic meningitis along with the product breakdown during desquamation of epithelial cells [5]. A possible substitute approach that avoids the invasiveness of an open craniotomy and the issues involved with shunting is neuroendoscopic treatment. Numerous research, including some instances, covers the use of endoscopy in the management of cerebral arachnoid cysts. Some authors prefer subtotal epidermoid cyst removal to avoid complications and patient morbidity [6]. In this case, we report the management of lateral ventricle ependymal lined neuroglial cysts using cystoventriculostomy and lower VP shunt procedures.
Patient information: a 79-year-old male with an acute decrease in consciousness, dysphagia, and seizures on antiepileptic drugs with a past medical history of a cystic mass in the frontal lobe. Comorbid patients with pulmonary Ca, coronary heart disease with a history of CABG. Had a history of diabetes mellitus in the last 25 years of using anti-diabetic drugs. Now patient was bedridden and hospitalized with pneumonia.
Clinical findings: we discovered a Glasgow Coma Scale (GCS) of 113, an anisochore pupil, hypertonic all extremities, and left lateralization with normal pathological reflex on physical examination. A chest X-ray revealed infiltate penumonia, and an MRI revealed a cystic lesion with calcification component in the left frontal lobe, a suspect ependymal lined neuroglial cyst, and a DD arachnoid cyst ECG: Atrioventricular reentrant tachycardia, T-Inverted lead II, III (Inferior Ischemia), laboratory findings leucocytosis, hyperglycemia, severe hypnonatremia. The patient has metabolic and septic problems, and we got interdisciplinary management with join care to Internist, pulmonologist, and cardiologist to stabilize the patient´s condition.
Diagnostic assessment: a CT scan of the head revealed a cystic lesion with the rim of calcification in the left frontal lobe, chronic lacunar infarction of the left internal capsule genu, left thalamus, senile brain atrophy, and moderate hydrocephalus (Figure 1).
Therapeutic interventions: the patient was scheduled for endoscopic cyst fenestration and low-pressure VP shunt. On MRI showed intraaxial cyst lesion with calcification and no enhancement after contrast. Endoscopic-cystoventriculotomy (cyst-fenestratum) with concurrent VP shunting was the chosen procedure in this patient, The burrhole was packed around the working sheath with wet cottonoids as soon as the cyst was entered with theworking sheath (Figure 2). Additionally, the in-and-out flow channels of the endoscope were closed, and the working channel was blocked by the insertion of the Hopkins scope. The cysts were inspected with the scopes.
Follow-up and outcome of interventions: the cyst wall relief resembled the typical cortical relief and did not include any identifiable landmarks in any case and (Figure 2) showed the Monroe foramen and plexus choroideus. The cystoventriculostomy was effortlessly carried done at the optimal perforation point using the method indicated (Figure 2) using the perforation forceps, the stoma was widened following the initial perforation until an open stoma of 4-5 mm in diameter was produced (Figure 2). The effective completion of the cystoventriculostomy was verified following the procedure by examining the ventricle through the stoma with the 0° diagnostic scope (Figure 2). There was no stent inserted. The bur hole was filled with Gelfoam after the working sheath was removed, and the wound was then firmly stitched, ensuring that there was no CSF leak. Postoperative Clinical Status presents that there were no immediate durante and postoperative complications, head CT-scan evaluation proven enhanced hydrocephalus and cyst size. Clinically patients were improved with decreased seizure frequency and intracranial pressure. But unfortunately, the patient is dead 5 months post-procedure because of an underlying disease. The patient had follow-ups after surgery for as long as 5 months. Patients who suffered from seizures ceased having seizures, and none are being treated with any anticonvulsant medication. A further decrease in cyst size was observed in these patients during follow-up. A significant decrease in cyst size at a 5-month follow-up is illustrated in Figure 3, Figure 4.
Patient perspective: as long as the patient is treated, the patient was delighted with the care and good service he received. He was optimistic that his condition will recover as before.
Informed consent: the patient´s family was informed about the report, why his case was peculiar. He gave informed consent to allow the authors to use his case for this case report.
The best course of treatment, which may involve microsurgical, endoscopic, or shunt implantation procedures, is still up for debate. The confidence in endoscopic procedures has increased recently due to the continued development and enhancement of endoscopic neurosurgery techniques [7]. Endoscopic treatment of arachnoid cysts appears to be substantially more common in the current literature, with additional data on open microsurgical procedures. A transcortical transventricular approach can be used to remove lesions from the anterior horn. Lesions that are caudally situated may be treated using the subtemporal approach. Cysts touching the choroid fissure and temporal horn were transcallosal. Abdominal crisis may develop from ventriculoperitoneal shunts through cerebral epidermoids. These lesions must be surgically removed with a well-positioned craniotomy, and the operative exposure depends on the topographical location within the lateral ventricle (atrium, temporal horn, etc.) [4].
The patient's head is positioned to enable for the cyst to be as close to the patient as feasible in a straight line (in this case, paraventricular cyst). The ideal location for the surgical incision can be found using stereotactic image guidance. The specified place of insertion is covered with a 2-cm linear incision. The region is covered by a burr hole. A tiny cortical incision is made to introduce a peel-away sheath into the ventricular cavity (Figure 4). Typically, the cyst wall is visible from an endoscopic view once the endoscope is inserted through the peel-away sheath [4]. A small opening in the cyst wall is next created using endoscopic forceps and scissors, and then it is widened using a double-balloon catheter. Before making an incision in the cyst wall, cautery might be utilized when the surface is vascularized. For cysts to be able to drain into a ventricle or a CSF cistern, there must be a large enough aperture. Utilizing an endoscope makes it possible to see the cyst's contents, pinpoint the location of the cyst's fenestration, and prevent damaging vital neurovascular structures.
Risk and benefit cyst fenestration lateral ventricle: a few studies looked into lateral ventricle cyst fenestration issues, however a study of ETV difficulties found that the total complication rate was 8.8%. There was 2.1% permanent morbidity, 1.2% neurologic morbidity (hemiparesis, gaze palsy, memory problems, and/or altered consciousness), and 0.9% hypothalamic morbidity (diabetes insipidus, weight gain, or precocious puberty) [8]. Intraoperative bleeding occurred in 3.9% of cases and was severe in 0.6% (including 4 cases (0.14%) of basilar rupture). Other surgical complications occurred in 1.13% of patients (3 thalamic infarcts, 6 subdural, 6 intracerebral, and 2 epidural hematomas). 1.8% of cases had CSF infections, 1.7% had CSF leaks, and 0.19% had anesthetic complications (bradycardia and hypotension). A different research team found two intraventricular hemorrhages and one thalamic damage, which are both significant consequences. Additional stitches may be used to stop the CSF leaks, and antibiotics are required to treat any CSF infections [8].
Craniotomy with direct cyst fenestration or cyst shunting is the best treatment for arachnoid cysts of the brain convexity and interhemispheric area (Table 1). The cyst can be fenestrated into the lateral ventricle using only endoscopic techniques; however, fenestration into the surrounding subarachnoid spaces is difficult, if not impossible, because these spaces are squeezed and nearly totally obliterated [9]. The clinicall outcome in this patient was a significant improvement, with less seizure frequency and a decrease of in intracranial pressure. There were only minor complications, including intraventricular hemorrhagic and CSF leakage. The surgical technique for neuroglial cysts (glioependymal cysts) using an endoscopic cyctoventriculostomy approach potentially work since the endoscopy can offer better intraoperative visualization and reduce patients' postoperative discomfort. Ependymal neuroglial cyst located lateral to the atrium and temporal horn to the ventricle lobes are appropriate justifications for surgery using this endoscopic cyctoventriculostomy approach. Ependymal cysts are nonenhancing periventricular neuroepithelial cysts that are coated by ependymal cells [10]. Similarly, [2] for symptomatic patients who presents with an ependymal neuroglial cyst, the treatment is surgical. Spite of the fact that their possible options, Neuroendoscopic cyst fenestration is a minimally invasive procedure with low morbidity, a short hospital stay, and long-term efficacy [11].
Overall, endoscopic cystoventriculostomy is the surgery of choice for ependymal lined paraventricular epidermoid cysts in our opinion. The technique should be preferred for the placement of a cystoventricular or cystoperitoneal shunt. The approach, trajectory, and site of fenestration must be carefully planned and studied intraoperatively in each instance using preoperative MR imaging. The cyst's location, on the other hand, is critical for surgical decision-making.
The authors declare no competing interests.
Farhad Bal'afif, Donny Wisnu Wardhana, Tommy Alfandy Nazwar, Achmad Bayhaqi Nasir Aslam, Ulil Abshor Ike Sulistiyowati and Mustofa Mustofa were responsible for the diagnosis and clinical management of the patient. Farhad Bal'afif and Achmad Bayhaqi Nasir Aslam responsible for surgical procedure. Ike Sulistiyowati and Ulil Abshor diagnosed the radiology and neurology approaceh. Ulil Abshor, and Mustofa Mustofa drafted the manuscript. Farhad Balafif and Donny Wisnu Wardhana, Tommy Alfandy Nazwar participated in the analysis, supervision, writing of the original draft, reviewing and editing of the manuscript for intellectual content. All authors read and approved the final manuscript.
Table 1: result of the surgical procedure in cortical and interhemispheric cysts
Figure 1: head CT pre cyst fenestration concomitant VP-shunt procedure
Figure 2: A) temporal muscle detaches and the muscle tacked down to the bone flap and bone drilled: B) insertion of endoscopic to cyst space; C) the Foramen Monroe and plexus choroideus were inspected for scopes; D) cystoventriculostomy immediately after perforation of the cyst wall; E) the stoma was enlarged by the use of the perforation forceps; F) cystoventriculostomy was checked by inspection of the ventricle through the stoma with the diagnostic scope
Figure 3: A) head CT-scan before fenestratum procedure; B) head CT-scan post fenestratum prosedure
Figure 4: head MRI without contrast
- Gankpé GF, Ndekha GJ, Okacha N, Chakour K, Chaoui MEF, Benzagmout M. Intracranial ependymal cyst with unusual presentation: Case report and review of literature. Interdiscip Neurosurg. 2019 Sep;17:45-8. Google Scholar
- Mustapha O, Allali N, Latifa C, El Haddad S. Epilepsy as a Presentation of a Neuroglial Cyst Associated with Dysgenesis of Corpus Callosum in a Child. Case Rep Radiol. 2021;2021:6675071. PubMed | Google Scholar
- Obaldo RE, Shao L, Lowe LH. Congenital glioependymal cyst presenting with severe proptosis. AJNR Am J Neuroradiol. 2007 Jul;28(6):999-1000. PubMed | Google Scholar
- Bhatoe HS, Mukherji JD, Dutta V. Epidermoid tumour of the lateral ventricle. Acta Neurochir (Wien). 2006 Mar;148(3):339-42; discussion 342. PubMed | Google Scholar
- De Decker S, Davies E, Benigni L, Wilson H, Pelligand L, Rayner EL et al. Surgical treatment of an intracranial epidermoid cyst in a dog. Vet Surg VS. 2012 Aug;41(6):766-71. PubMed | Google Scholar
- Akar Z, Necmettin TanRiover, Saffet Tuzgen, Ali M. Kafadar and Cengiz Kuday. Surgical Treatment of Intracranial Epidermoid Tumors. Nuerol Med Chir (Tokyo). 2003;43, 275-281. PubMed | Google Scholar
- Oertel J, Vulcu S, Eickele L, Wagner W, Cinalli G, Rediker J. Long-Term Follow-Up of Repeat Endoscopic Third Ventriculostomy in Obstructive Hydrocephalus. World Neurosurg. 2017 Mar 1;99:556-65. PubMed | Google Scholar
- Yadav YR, Parihar V, Pande S, Namdev H, Agarwal M. Endoscopic third ventriculostomy. J Neurosci Rural Pract. 2012 May;3(2):163-73. PubMed | Google Scholar
- Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F. Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr. 2011 Aug;8(2):158-64. PubMed | Google Scholar
- Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006 Jun;239(3):650-64.. PubMed | Google Scholar
- Alvarado AM, Smith KA, Chamoun RB. Neuroendoscopic fenestration of glioependymal cysts to the ventricle: report of 3 cases. J Neurosurg. 2019 Nov;131(5):1615-9. PubMed | Google Scholar
Search
This article authors
On Pubmed
On Google Scholar
Citation [Download]
Navigate this article
Similar articles in
Key words
Tables and figures
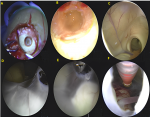 Figure 2: A) temporal muscle detaches and the muscle tacked down to the bone flap and bone drilled; B) insertion of endoscopic to cyst space; C) the Foramen Monroe and plexus choroideus were inspected for scopes; D) cystoventriculostomy immediately after perforation of the cyst wall; E) the stoma was enlarged by the use of the perforation forceps; F) cystoventriculostomy was checked by inspection of the ventricle through the stoma with the diagnostic scope
Figure 2: A) temporal muscle detaches and the muscle tacked down to the bone flap and bone drilled; B) insertion of endoscopic to cyst space; C) the Foramen Monroe and plexus choroideus were inspected for scopes; D) cystoventriculostomy immediately after perforation of the cyst wall; E) the stoma was enlarged by the use of the perforation forceps; F) cystoventriculostomy was checked by inspection of the ventricle through the stoma with the diagnostic scope