A standardised neonatal admission record (NAR) - increasing quality of neonatal care in Rwanda-a retrospective observational study
Jaeseok Choi, Raban Dusabimana, Fedine Urubuto, Faustine Agaba, Daniel Langer, Catherine Harrison, Cliff O’Callahan, Peter Thomas Cartledge
Corresponding author: Peter Thomas Cartledge, Department of Pediatrics, University Teaching Hospital of Kigali (CHUK), Kigali, Rwanda 
Received: 18 Feb 2020 - Accepted: 16 Mar 2020 - Published: 27 Apr 2020
Domain: Health communication,Pediatrics (general)
Keywords: Infant, newborn, mortality, medical records, developing countries, Rwanda
©Jaeseok Choi et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Jaeseok Choi et al. A standardised neonatal admission record (NAR) - increasing quality of neonatal care in Rwanda-a retrospective observational study. PAMJ Clinical Medicine. 2020;2:161. [doi: 10.11604/pamj-cm.2020.2.161.21853]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/2/161/full
Research 
A standardised neonatal admission record (NAR) - increasing quality of neonatal care in Rwanda-a retrospective observational study
A standardised neonatal admission record (NAR) - increasing quality of neonatal care in Rwanda-a retrospective observational study
Jaeseok Choi1,2, Raban Dusabimana1,2, Fedine Urubuto1,2, Faustine Agaba 2, Daniel Langer3,4, Catherine Harrison3,5, Cliff O´Callahan6, Peter Thomas Cartledge2,7,8,&
1School of Medicine, University of Rwanda, Kigali, Rwanda, 2Department of Pediatrics, University Teaching Hospital of Kigali (CHUK), Kigali, Rwanda, 3Birthlink (UK Charity), Ickenham, Middlesex, United Kingdom, 4Department of Pediatrics, Epsom and St Helier University Hospitals NHS Trust, London, United Kingdom, 5Department of Neonatology, Leeds Children´s Hospital NHS Trust, Leeds, United Kingdom, 6Department of Pediatrics, Middlesex Health and University of Connecticut, Connecticut, USA, 7Department of Emergency Medicine, Yale University, New Haven, USA, 8Rwanda Human Resources For Health (HRH) Program, Ministry of Health, Kigali, Rwanda
&Corresponding author
Peter Thomas Cartledge, Department of Pediatrics, University Teaching Hospital of Kigali (CHUK), Kigali, Rwanda
Introduction: the neonatal period is the most vulnerable time for a child´s survival. It is well established that high-quality medical records are needed for the provision of high-quality care and that neonatal medicine is well suited to a standardised approach to care. The objective of this study was to describe the implementation of a Neonatal Admission Record (NAR) and to retrospectively compare discharge outcomes (length of hospital stay, mortality and weight gain) for neonates born before and after implementation.
Methods: a retrospective observational study was undertaken. A NAR was implemented, in combination with an education package, in an urban, tertiary neonatal unit in Kigali, Rwanda. Length of stay, mortality and weight gain were compared before and after the implementation of the NAR.
Results: five hundred and fifteen pre-NAR and 863 post-NAR cases were included. There was a small, non-significant, increase in the mean LoS from 13.7 to 14.2 days. All-cause mortality decreased from 22% to 18% after the implementation of the NAR (OR=0.76, p=0.049). Surviving neonates gained 4.1 and 6.1g/kg/day before and after the implementation of the NAR (p=0.031).
Conclusion: the use of a standardised Neonatal Admission Record, in combination with an educational package, can improve care. A NAR provides a structured approach to managing infants on a neonatal unit in the resource-limited setting.
Neonatal mortality: the neonatal period is the most vulnerable time for a child´s survival, yet, globally, from 1990 to 2016 the decline in neonatal mortality (49%) has been slower than mortality for children under-5 (62%) [1,2]. Three-quarters of neonatal deaths happen in the first week with the highest risk of death on the first day of life [3]. The majority of neonatal deaths (99%) occur in resource-limited countries [3]. Simple, cost-effective interventions are therefore required, including education and training and integrated service delivery packages, such as skilled birth attendants in dedicated birth centres.
Standardised hospital records for neonates: one simple, potentially cost-effective, intervention is standardised hospital admission records to document the entire hospital stay. It is well established that high-quality medical records are needed for high-quality care. The importance of accurate record keeping and data collection has led the World Health Organization (WHO) to produce a manual for developing standardised medical records, as well as a guide for developing countries on improving data quality [4,5]. Healthcare professionals (HCPs) need information, at the point of service, and at the point of decision making. This information should be in a format that maximises the decision-making process. The WHO states that accurate and reliable medical records are imperative for enabling continuous care of patients at all levels of healthcare. They are also an essential medico-legal record. There are several benefits to standardised medical records: they are a key tool used to improve patient care by assisting clinical decision making and management throughout the admission, and in doing so, provide education and act as an aide-memoire to HCPs [6,7]. When documentation is adequately performed, it can improve the coordination and continuity of care, reinforce clinical decision-making capacities, achieve more accurate statistical data and augment staff accountability [8-10].
On a larger scale, a standardised medical record can also act as a source of data for service activity reporting, performance monitoring of hospitals and for audit, research and education [11,12]. Following a review of multiple audits of medical record keeping in the United Kingdom (UK), the UK´s Audit Commission proposed the development of medical note folders with standards for structure and content [13]. A review in the Lancet in 1998 by Wyatt et al, reported that structured notes supported clinical decision making [14]. They also help to limit errors, improve understanding and interpretation of management plans resulting in improvements in patient outcomes and reduction in costs [15]. There is a paucity of national and international data available for many neonatal intervention programmes in low-income countries (LICs) due to the lack of data collection and accurate or specific documentation [11,16]. Simple, low-cost interventions such as standardised Neonatal Admission Records (NAR) are one-step in the process required to improve and document care provision, improve the communication between HCPs and to aid data collection. Indirectly, there is the potential that they could improve patient management and therefore overall morbidity and mortality.
Aims: there is currently no literature on the effectiveness of standardised admission records on quality of care in neonatology. The objective of this study was to describe the implementation of a Neonatal Admission Record (NAR) and to retrospectively compare discharge outcomes (length of hospital-stay, mortality and weight gain) for neonates born before and after implementation.
Study design: a retrospective observational study to assess the implementation of a NAR. Reporting of this study has been verified in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist [17].
Location: the neonatology unit of the University Teaching Hospital of Kigali (CHUK). CHUK is the largest, public, tertiary referral hospital in Rwanda, located in Kigali city, and also serves as a teaching hospital for the University of Rwanda. CHUK is a referral centre for high-risk pregnancies and deliveries and cares for approximately 2000 deliveries annually; the neonatal unit has approximately 560 admissions annually [18].
The BirthLink NAR: BirthLink is a UK based charity, supporting neonatal care provision in the region. In early 2012 it was identified that medical records on the neonatal unit were scarce, and medical clerkings used generic admission proformas that represented the medical history of an older child or an adult which were inappropriate for a neonate. Therefore, the BirthLink team collaborated with local HCPs to produce a detailed NAR. The items and structure of the NAR was based on the NAR from members of the BirthLink team and the Emergency Triage, Assessment and Treatment (ETAT) resources from Kenya [19,20]. The NAR was implemented with the aim of providing structure to admissions and ward-rounds, informing HCPs of what specific examination and management plans needed to take place, in a sub-speciality where nursing and junior clinical staff may not be neonatal trained. The NAR was designed to align with national neonatal guidelines and to improve communication between doctors, nurses and parents, providing accurate data for future audit and feedback. The purpose of the NAR was to aid HCPs working in the neonatal unit to deliver and document care.
Major confounders: the introduction of the NAR was introduced concurrently with a neonatal training package provided by a collaboration of Imperial College (London, UK), The Tropical Health and Education Trust (UK) and BirthLink Charity (UK) and the introduction of bubble CPAP to four neonatal units across Rwanda from March 2012. In April 2012 the BirthLink Charity (UK) facilitated the introduction of CPAP into the unit. The Birthlink education package included training on thermal control, feeding and infection prevention as well as the introduction of non-invasive respiratory support. The NAR facilitated implementation of the education package and guided and documented the use of CPAP as well as other aspects of neonatal care. In August 2012 the US-funded Human Resources for Health program began which placed a new Rwandan paediatric graduate and a US paediatrician in the NICU to provide daily rounding supervision and reinforcement use of the NAR [21,22]. Quality improvement programs were implemented, using the NAR as a guide, to initiate weekend rounding and routine vital sign measurements on every shift, plot growth, and encouraging residents to advance feeding according to the guidelines in the aforementioned trainings.
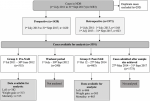
The CHUK neonatal database (NDB): the CHUK neonatal database (registry) was established in 2013 and the description of its development has been described in the literature [18,23-26]. All admitted neonates are included in the CHUK NDB either prospectively or retrospectively. The NDB was not explicitly established to monitor the NAR and is rather used for research, audit and feedback purposes: Prospective collection: data was collected prospectively, using a paper data-collection form from 1st July 2013. Pediatric residents on-duty for the neonatal unit completed the data collection. Residents are encouraged to actively complete the process during the admission of the neonate. However, our experience suggests that many forms are completed at the point of discharge. Data is then inputted from the paper data collection form onto the CHUK "Neonatal Database (NDB)" (registry) using Microsoft Access on a password-protected laptop. Retrospective collection: data was inputted entirely retrospectively from 1st July 2011 to 1st July 2013 from the Ministry of Health (MoH) nursing admission book. After this period the MoH nursing admission book for the neonatal unit was reviewed retrospectively to identify any missing cases that had not been enrolled prospectively. These missing cases were added retrospectively to the NDB using simple data (gestation, birth weight, mortality) from the nursing admission book (Figure 1). This data does not include CPAP use and therefore no measurement of the CPAP confounder was possible. Data quality: data on subjects was not always complete. For example, to calculate daily weight gain, four data items were required, namely; admission weight, discharge weight, admission date and discharge date. If one data point was absent, then the outcome could not be measured or described.
Recruitment/enrolment of participants: all neonates admitted in the newborn care unit are included and entered into the NDB at the point of discharge.
Participants/subjects: the NAR was introduced at CHUK in July 2012. In this study, we have used a three month "wash-out period" which we have not included in the analysis to allow for transition on to the new NAR. The pre-NAR neonates were recruited in the months before and including June 2012 when the NAR was introduced. The post-NAR neonates were recruited three months after the introduction of the NAR, i.e. after November 2012. Two groups of patients were therefore included in the analysis between the 1st July 2011 and the 13th October 2013 (n=1280): group 1: NAR not in use (pre-30th June 2012); Group 2: NAR in use (post-1st Oct 2012). The “Washout period” to allow for transitioning to use of NAR from 30th June 2012 until 30th Sept 2012 (3 months) was not included in the analysis.
Variables and outcomes: the primary outcome was the length of stay (LOS). The secondary outcomes were discharge weight and mortality.
Sample size (power calculation): the NDB contained data available on 515 neonates before the introduction of the BirthLink NAR (Figure 1). These contained sufficient details to provide data on length of stay (LOS) (n=382). For a 20% change in LOS with 95% confidence and 80% power, sample sizes of pre-NAR (n=343) and post-NAR (n=686) would be required.
Ethics/Study Oversight: Funding & Sponsors: no funding has been sought for this project. The laptop for the NDB was a donation from Middlesex Hospital, Middletown, Connecticut, USA. No funding has been sought for the analyses of the neonatal database analysis. The neonatal NAR was funded, designed and implemented by BirthLink, a UK charity working in Rwanda and the Democratic Republic of Congo, led by Kathy Mellor (KM). Confidentiality: the laptop is kept in a locked cabinet/office and is password protected. Names or other patients' identification information was not disclosed publicly. Informed consent: data is routinely collected in the database for the quality of care monitoring. As this is for service review with no experimentation on subjects; informed consent was not necessary or undertaken. Incentives for subjects: subjects did not receive any incentive for this study. Risk to subjects (including safeguards to mitigate these risks): Although every study carries some degree of risk to participants, there were no significant physical, legal, financial, emotional and/or social risks to the subjects identified during this study. Institutional Review Board (IRB): the project proposal was approved by the CHUK Research Ethics Committee (REC). Ref: REC/CHUK/204/2017.
Statistical analysis: data were analysed using Statistical Package for the Social Sciences (SPSS) version 24. Categorical data was described in ordinal tables and analysed with Chi-square and Fisher´s exact test when cells had less than five cases. These bivariate analyses were presented with p-values and Odds-Ratios (OR). Continuous data were described using means and compared with Student´s t-test or ANOVA dependent on group size.
Participants: the NDB contained 3391 cases available for analysis (Figure 1). Cases with missing data points were excluded. Pre-NAR (n=515) and post-NAR (n=863) cases were included in order to achieve the pre-defined sample size for the primary outcome of length of stay. Neonates admitted in the three-month washout period (n=240) were not included in the analysis. There were no significant differences in gender, birth weight, birthplace (in or out) gestation and rates of SGA between the pre- and post-NAR groups (Table 1).
Length of stay: the study was powered to assess for a 20% change in LoS. There was a small, non-significant, increase in the mean LoS from 13.7 to 14.2 days after the introduction of the NAR (Table 2).
Weight gain: weight gain was calculated for surviving infants. Weight gain was calculated from the admission and discharge weight and therefore includes the initial drop in weight found in neonates. Surviving neonates gained 4.1 and 6.1g/kg/day before and after the implementation of the NAR (p=0.031, Table 2).
Mortality: all-cause mortality decreased from 22% to 18% after the implementation of the NAR (OR=0.76, p=0.049, Table 2).
The objective of this study was to retrospectively compare discharge outcomes (length of hospital-stay, mortality, and weight gain) for neonates born before and after the implementation of a standardised Neonatal Admission Record (NAR). We have shown a reduction in mortality and an improvement in weight gain in surviving neonates. There was no significant change in LoS.
Documentation: several studies have looked at the paucity of documentation and its effect on care. However, lack of data, both qualitative and quantitative, can make it difficult to assess the quality of care delivered [27]. Studies looking at the quality of neonatal healthcare in Tanzania and Papua New Guinea showed that care was affected by poor documentation and a lack of standard systems for documentation across facilities [28,29]. The lack of this standardised system affected recording medical assessments and management plans. The authors describe that written information was minimal and key diagnoses, such as prematurity, were missing in a substantial proportion of notes. The authors concluded that training, motivation and standardised guidelines were needed to improve the quality of care alongside dedicated standardised medical records.
Neonatal care: neonatal care is highly organised speciality and therefore well suited to a standardised structure. It is postulated that by having the same daily proforma, the clinical team can learn and deliver a systematic approach in order to standardise ward rounds and management plans. By having tick boxes allows a non-biased method of data collection and also an easily legible method of analysis.
Education: by running simultaneous training programmes, there is evidence to suggest that this “blended learning” approach can make the process of change to a new system easier and that this should be maintained through monitoring and reinforcement [30]. We felt therefore, it was appropriate to introduce the NAR at the same time as a neonatal training programme for doctors and nurses on the neonatal unit with the aim of enhancing care provision. By introducing neonatal training to medical and nursing staff, and introducing systematically structured ward-rounds and documentation, HCPs can have a better understanding of the management of the sick infants under their care. Having a NAR proforma that clearly describes and presents this process of care also acts as an aide memoir to prevent omission of essential aspects of care. For example, before the implementation of the NAR, many infants spent prolonged periods on intravenous fluid, being deprived enteral nutrition due to a fear of feeding causing Necrotising Enterocolitis (NEC). In our NAR, the proforma prompts the HCP to consider all aspects of enteral feeding and therefore to advance feeds appropriately. This prompt, used daily by the rounding attendings to guide rotating groups of students and residents, could have been the factor that contributed to the significant improvement in weight gain in admitted neonates. The NAR was modified during the first year of use based on feedback from the on-site team. The importance of local on-site champions for NAR implementation must be emphasized: the record was not introduced in other teaching sites, despite interest, until required by the Ministry. Even at CHUK, where this was introduced and championed, it is currently not being used for neonates admitted on wards outside of the NICU.
Benefits of neonatal admission records: the benefits measured in this study are limited to LoS, mortality and weight gain. However, there are many other benefits, which have not been described in the literature. These include enhanced data-collection for research and quality improvement projects, and reduced time to document care with tick-box completion. Use of the Rwandan NAR instigated the small unit-specific quality improvement program that quickly led to vitals being recorded at every shift, growth charts being plotted weekly, orders being acknowledged by nurses, and rounds and orders occurring on weekends.
Neonatal registries: globally, many neonatal units are now employing databases (registries) to allow for benchmarking against similar units [11,31]. Registries have the purpose of monitoring quality of care, providing feedback, benchmarking performance, describing the pattern of treatment, reducing variation and as a tool for conducting research [32,33]. The quality of the data inputted into registries is frequently dependent upon the quality of documentation in patient files. Therefore, a NAR has the potential to not only improve care of each individual neonate but also to contribute to systems for improvement, such as registries. Without the NAR it would have been unfeasible for our unit to develop our registry to monitor quality [18].
Confounders and limitations of the study: the NAR was introduced with an education programme covering thermoregulation, infection control, KMC and respiratory care. The NAR supported the principles of education provided. The NAR and education package were interlinked and support each other. The NAR and the neonatal database were designed independently and by different groups. Therefore, the outcomes used to assess the use and effectiveness of the NAR were not complete. For example, outcomes such as “employee time” to complete the NAR were not assessed. Our study does not quantify the quality (completeness) of documentation that was undertaken before and after the introduction of NAR. CPAP was introduced concurrent with the introduction of the NAR. it is certainly feasible that the use of CPAP within the education package could account for some of the benefits seen. Finally, the timescale within which it took to recruit the post-NAR group was twice as long as the pre-NAR group and therefore general improvements in care, such as the presence of trained paediatricians conducting daily rounds and reinforcing the use of the NAR and neonatal protocols, could account for the results.
The introduction of a standardised Neonatal Admission Record (NAR), alongside an education and implementation programme, can significantly improve outcomes in a low-resource setting.
What is known about this topic
- Standardised medical records are a key tool used to improve patient care.
What this study adds
- A standardised Neonatal Admission Record has been a key component of improving care in one tertiary hospital in Rwanda.
The authors declare no competing interests.
All authors confirm that they have made substantial academic contributions to this manuscript as defined by the ICMJE. The project was undertaken as a final-year research project for the Medical Degrees (MD) of three authors (JC, FI, RD), supervised by the corresponding author (PC). The neonatal database was instituted by CO. Data-collection was undertaken and supervised by JC, FI, RD & FA. The NAR was designed and implemented by the BirthLink team (CH, DL). All authors contributed to the final manuscript
We acknowledge the significant input of the BirthLink charity and in particular the work of Kathy Mellor.
Table 1: baseline database
Table 2: outcomes
Figure 1: patient flow chart
- UNICEF. The neonatal period is the most vulnerable time for a child. 2018. Accessed 13 June 2018.
- World Health Organisation. Children: reducing mortality. Accessed 13 June 2018.
- Lawn JE, Cousens S, Zupan J. Neonatal Survival 14 million neonatal deaths: When? Where? Why?. Lancet. 2005;365(9642):891-900. PubMed | Google Scholar
- World Health Organization (WHO). Medical Records Manual: a guide for developing countries. WHO. 2006. Google Scholar
- World Health Organisation (WHO). Improving Data Quality: a guide for developing countries. WHO. 2003;1-74. Google Scholar
- Snell P. Writing it down. Br Med J. 1984;289(6459):1674-8. PubMed | Google Scholar
- Pourasghar F, Malekafzali H, Kazemi A, Ellenius J, Fors U. What they fill in today, may not be useful tomorrow: Lessons learned from studying Medical Records at the Women hospital in Tabriz, Iran. BMC Public Health. 2008;8:139. PubMed | Google Scholar
- Pirkle CM, Dumont A, Zunzunegui MV. Medical recordkeeping, essential but overlooked aspect of quality of care in resource-limited settings. Int J Qual Heal Care. 2012;24(6):564-567. PubMed | Google Scholar
- Williams F, Boren S. The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. Inform Prim Care. 2008;16(2):139-145. PubMed | Google Scholar
- Wong R, Bradley EH. Developing patient registration and medical records management system in Ethiopia. Int J Qual Heal Care. 2009;21(4):253-258. PubMed | Google Scholar
- Maina M, Aluvaala J, Mwaniki P, Tosas-Auguet O, Mutinda C, Maina B et al. Using a common data platform to facilitate audit and feedback on the quality of hospital care provided to sick newborns in Kenya. BMJ Glob Heal. 2018;3(5):e001027. PubMed | Google Scholar
- Royal College of Physicians. Why standardise the structure and content of medical records. AoMRC. 2008;1-16.
- Nicholson L. Setting the records straight: a study of hospital medical records undertaken by the Audit Commission. Rec Manag J. 2005;6(1):13-32. Google Scholar
- Wyatt JC, Wright P. Medical records Design should help use of patients´ data. Lancet. 1998;352(9137):1375-1378. PubMed | Google Scholar
- Wright P, Jansen C, Wyatt JC. Medical records How to limit clinical errors in interpretation of data. Lancet. 1998;352(9139):1539-43. PubMed | Google Scholar
- UNICEF. Tracking progress towards universal coverage for women´s, children´s and adolescents´ health The 2017 Report. UNICEF. 2017.
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. PubMed | Google Scholar
- Choi J, Urubuto F, Dusabimana R, Kumwami M, Agaba F, Teteli R et al. Establishing a neonatal database in a tertiary hospital in Rwanda-an observational study. Paediatr Int Child Health. 2019;39(4):265-274. PubMed | Google Scholar
- Kenya Paediatric Association. Neonatal Admission Record (Kenya), Emergency Treatment Assessment and Triage (ETAT+), Neonatal Admission Record. 2017. Accessed 21 April 2020.
- Kenya Paediatric Association (KPA). Emergency Triage Assessment and Triage - Feeding & Weight Chart. KPA. 2019.
- Cancedda C, Cotton P, Shema J, Rulisa S, Riviello R, Adams L V et al. Health Professional Training and Capacity Strengthening Through International Academic Partnerships: The First Five Years of the Human Resources for Health Program in Rwanda. Int J Heal Policy Manag. 2018;7(11):1024-1039. PubMed | Google Scholar
- Mccall N, Umuhoza C, Callahan CO, Rogo T, Stafford D, Kanyamuhunga A et al. Measuring change in knowledge acquisition of Rwandan residents?: using the American Board of Pediatrics International In-Training Examination ( I-ITE ) as an independent tool to monitor individual and departmental improvements during the Human Resources f. BMC Med Educ. 2019;19(217):1-9. Google Scholar
- Urubuto F, Agaba F, Choi J, Dusabimana R, Kumwami M, Conard C et al. Prevalence, risk factors and outcomes of neonatal hypothermia at admission at a tertiary neonatal unit, Kigali, Rwanda-a cross-sectional study. J Matern Neonatal Med. 2019;1-8. PubMed | Google Scholar
- Cartledge P, Iratubona, Dusabimana, Choi, Agaba, Teteli et al. Hypothermia prevalence and risk factors in admitted neonates and impact on outcomes at a tertiary neonatal unit, Rwanda: a crosssectional study. Arch Dis Child. 2019;104(Supplement 2):A107. Google Scholar
- Cartledge P, Dusabimana R, Choi J, Iratubona F, Agaba A, Teteli R et al. Characteristics and outcomes of small for gestational age (SGA) neonates at a tertiary hospital neonatal unit in Rwanda: a cross-sectional study. Arch Dis Child. 2019;104(Supplement 2):A110-A111. Google Scholar
- Dusabimana R, Jaeseok C, Urubuto F, Agaba F, Teteli R, Kumwami M et al. Case-load, associated characteristics and outcomes of small for gestational age (SGA) neonates admitted to a tertiary hospital neonatal unit in Kigali, Rwanda: a cross-sectional study. Pan African Med J - Clin Med. 2020;1(64):1-12. Google Scholar
- Kidanto HL, Massawe SN, Nystrom L, Lindmark G. Analysis of perinatal mortality at a teaching hospital in Dar es Salaam, Tanzania, 1999-2003. Afr J Reprod Health. 2006;10(2):72-80. PubMed | Google Scholar
- Mbwele B, Reddy E, Reyburn H, Mbwele B, Reddy E, Reyburn H et al. A rapid assessment of the quality of neonatal healthcare in Kilimanjaro region, northeast Tanzania. BMC Pediatr. 2012;12:182. PubMed | Google Scholar
- Nasi T, Vince JD, Mokela D, Moresby P, Hospital G, Sciences H et al. Mortality in children admitted to Port Moresby General Hospital: how can we improve our hospital outcomes?. P N G Med J. 2003;46(3-4):113-124.. PubMed | Google Scholar
- Mann R, Williams J. Standards in medical record keeping. Clin Med. 2003;3(4):329-32. PubMed | Google Scholar
- University of Vermont. Improving Care for Newborns Around the World. Accessed 21 April 2020.
- Hoque DE, Kumari V, Hoque M, Ruseckaite R, Romero L, Evans SM. Impact of clinical registries on quality of patient care and clinical outcomes: a systematic review. PLoS One. 2017;(September):1-20. PubMed | Google Scholar
- Gueye M, Gueye MN, Mbaye M, Abdoulaye M, Diouf A, Wade M et al. Crossing the Line to Electronic Medical Records in Subsaharian Africa: An Obstetric and Neonatal Information System with Perinatal Indicators Dashboard. J Heal Sci Res. 2017;12(9):e0183667. PubMed