High grade primary leiomyosarcoma of the mandible: case report and literature review
Ilias Benchafai, Leila Afani
Corresponding author: Ilias Benchafai, Service d’ORL, 5ème Hôpital Militaire, Geulmim, Maroc 
Received: 12 Dec 2019 - Accepted: 19 Jan 2020 - Published: 01 Feb 2020
Domain: Otolaryngology (ENT)
Keywords: Leiomyosarcoma, mandible, head and neck sarcomas, incidence, histology, treatment
©Ilias Benchafai et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Ilias Benchafai et al. High grade primary leiomyosarcoma of the mandible: case report and literature review. PAMJ Clinical Medicine. 2020;2:26. [doi: 10.11604/pamj-cm.2020.2.26.21295]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/2/26/full
High grade primary leiomyosarcoma of the mandible: case report and literature review
Ilias Benchafai1,&, Leila Afani2
1Service d´ORL, 5e Hôpital Militaire, Geulmim, Maroc, 2Service d´Oncologie Médicale, CHU Mohamed VI, Marrakech, Maroc
&Corresponding author
Ilias Benchafai, Service d´ORL, 5e Hôpital Militaire, Geulmim, Maroc
Leiomyosarcoma is a rare tumor derived from smooth muscle cells. Oral cavity location is uncommon and represents less than 1%. Only few cases were described in the mandible. Clinical and radiological findings are not specific. Diagnosis is based to histology. The main treatment is surgery and prognosis depend of the quality of resection. We report a clinical case of 33-year-old-woman with a month history of swelling in the left mandible. Computed tomography revealed an extensive lesion involving the left mandibular angle. Surgery with clear margins was not possible and chemotherapy followed by radiotherapy was given. The aim of this work is to review literature concerning this rare malignancy and discuss incidence, histology and treatment approaches.
Leiomyosarcoma is a malignant neoplasm of smooth muscle origin representing 7% of all soft issue sarcomas. These tumors are more common in gastrointestinal tract, uterus and retroperitoneal region [1]. Leiomyosarcoma represents only 4% of head and neck sarcomas [1]. Most reported sites of occurrence are maxillary sinus, mandible and maxilla. Other reported locations were tongue, lips and palate [2]. Clinically; it´s an aggressive tumor with a poor prognosis. The standard treatment is based on surgery. Because of scarcity of cases, there is no consensus regarding management of this tumor. By presenting this case, we propose a review of the literature concerning incidence, diagnosis and treatment options in this rare malignancy.
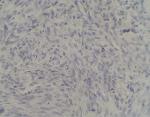
In July 2015, a 33-year-old woman without clinical antecedents presented with an 8 months history of a swelling in the left mandible. Clinical examination showed a diffuse left facial swelling and asymmetry without cervical lymphadenopathy (Figure 1). Computed tomography (CT) scans with contrast revealed an extensive lesion in the left mandibular angle responsible of bone lysis. It measuring about 64x58mm and extending to the height of 69mm (Figure 2).There was no regional lymphadenopathy and CT scan of chest, abdomen and pelvic were normal. A biopsy was performed. Histology showed intersecting fascicles of spindle cells (Figure 3 A, B).The cells have a high mitotic activity (13 per 10 high-power fields) with necrosis. No vascular emboli´s was observed. Immunohistochemical showed a positivity of vimentin, smooth-muscle-actin and H-caldesmone (Figure 4, Figure 5). EMA, cytokeratins, PS100 and CD 10 were all negative (Figure 6). And diagnosis of leiomyosarcoma of the mandible grade II FNCLCC was made. After a multidisciplinary medical opinions coordinaton, chemotherapy based on dacarbazine and doxorubicine was indicated. Assessment after three courses of chemotherapy, has demonstrated a stability of the disease. Surgery was excluded and radiotherapy was indicated.
Leiomyosarcoma is extremely rare in oral cavity and represents 0.06% of all neoplasms in this region [2]. This scarcity is due to paucity of smooth cell in this location. First case of mandibular leiomyosarcoma was described by Carmody in 1944 [3]. To our Knowledge, about 36 cases of primary leiomyosarcoma of the mandible have been published in English literature and we report an additional case of this rare malignancy. The median age is 34 years old with high incidence occurred in third and fourth decades. In the total of 36 cases reported 14 were male and 22 were female [4-8]. Clinically there are no specific presentations. These tumors can manifest as a painless or slowly enlarged mass. Using CT and Magnetic resonance imaging (MRI) are the way best to identify tumor extension [4]. Definitive diagnosis of leiomyosarcoma is based on histopathologic confirmation. Histologically, these tumors are characterized by spindle-shaped cells and presence of myofilaments, pinocytic vesicles, dense bodies and basal lamina. Malignant criterias to differentiate from leiomyoma are cellular atypia, necrosis and number of mitosis. In immunohistochemical analysis, positive desmin, vimentin, smooth-muscle-specific actin and H-caldesmon are the best indicator for leiomyosarcoma [9, 10]. Due to rarity of cases, treatment recommendations are derived from clinical trials conducted in extremity sarcomas. The main therapeutic approach of leiomyosarcoma is based on surgery. Hemimandibulectomy with a safety margins is the most important prognosis factor. Neck dissection is indicated if there is clinical evidence of metastasis lymph node [1]. However, the anatomical characteristic in head and neck make such radical surgery very difficult, allowing rarely free margins of resection. Moreover, such surgical approach should be exclusively dedicated to highly specialized ENT surgery team with high clinical expertise. Post-operative external radiotherapy is often indicated to improve local control [1]. Chemotherapy is indicated for unresectable or metastatic tumors [5]. The prognosis of leiomyosarcoma in the head and neck depends of the site, the extent of the primary tumor and the quality of resection [11].
Leiomyosarcoma of mandible is very rare. The lack of data from randomized clinical trials explains the complexity of the management of these tumors. Early diagnosis and aggressive surgery with safe margins is the only guaranty for the best prognosis.
The authors declare no competing interests.
All the authors have read and agreed to the final manuscript.
Figure 1: photograph shows massive swelling in the left side of mandible
Figure 2: axial cut of computed tomography showing heterogeneous mass in the left mandibular angle
Figure 3: A) photomicrocraph
shows fascicles of spindle cells with high mitotic activity and necrosis (magnification
x10); B) photomicrocraph shows fascicles of spindle cells with high mitotic
activity and necrosis (magnification x20)
Figure 4: photomicrograph showing positive immunoreactions for smooth muscle actin in the tumor cell
Figure 5: photomicrograph
showing positive immunoreactions for h-Caldesmon in the tumor cell
Figure 6: photomicrograph showing negative immunoreactions for CD 10 in the tumor cell
- Yadav J, Bakshi J, Chouhan M, Modi R. Head and neck leiomyosarcoma. Indian J Otolaryngol Head Neck Surg. 2013;65(Suppl 1):1-5. PubMed | Google Scholar
- Ethunandan M, Stokes C, Higgins B, Spedding A, Way C, Brennan P. Primary oral leiomyosarcoma: a clinico-pathologic study and analysis of prognostic factors. International Journal of Oral and Maxillofacial Surgery. 2007;36(5):409-416. PubMed | Google Scholar
- Carmody TE, Janney HM, Husesman HAL. Leiomyosarcoma of the mandible: report of case. The Journal of the American Dental Association. 1944;31(15):1110-1113. Google Scholar
- Ries Centeno C, Nadini F, Adam R, Godoy H, Reichart PA. Primary leiomyosarcoma of the mandible. Oral Oncology Extra. 2006;42(1):40-45. Google Scholar
- Singal D, Kamarthi N, Taneja N. Leiomyosarcoma of the mandible in a 15-year-old girl: a case report and a brief literature review of mandibular leiomyosarcomas. IJOMS. 2010;9(1):48-56. Google Scholar
- Rege ICC, Costa NL, Batista AC, da Silva CM, Meneghini AJ, Mendonça EF. High-grade primary leiomyosarcoma in the mandible: diagnosis and treatment. Head Neck. 2013;35(2):E44-E48. PubMed | Google Scholar
- Patel K, French C, Khariwala SS, Rohrer M, Kademani D. Intraosseous leiomyosarcoma of the mandible: a case report. Journal of Oral and Maxillofacial Surgery. 2013;71(7):1209-1216. PubMed | Google Scholar
- Moghadam SA, Khodayari A, Mokhtari S. Primary leiomyosarcoma of the mandible. J Oral Maxillofac Pathol. 2014;18(2):308-311. PubMed | Google Scholar
- Nikitakis NG, Lopes MA, Bailey JS, Blanchaert Jr RH, Ord RA, Sauk JJ. Oral leiomyosarcoma: review of the literature and report of two cases with assessment of the prognostic and diagnostic significance of immunohistochemical and molecular markers. Oral Oncology. 2002;38(2):201-208. PubMed | Google Scholar
- Watanabe K, Kusakabe T, Hoshi N, Saito A, Suzuki T. h-Caldesmon in leiomyosarcoma and tumors with smooth muscle cell-like differentiation: its specific expression in the smooth muscle cell tumor. Human Pathology. 1999;30(4):392-396. PubMed | Google Scholar
- Aljabab AS, Nason RW, Kazi R, Pathak KA. Head and neck soft tissue sarcoma. Indian J Surg Oncol. 2011 Dec;2(4):286-90. PubMed | Google Scholar