Emphysematous cystitis complicated by bladder rupture: a paraplegic patient case
Abdelghani Ouraghi, Amine El Houmaidi, Tarik Mhanna , Mohamed Irzi, Mehdi Chennouf, Anouar El Moudane, Ali Barki
Corresponding author: Abdelghani Ouraghi, Department of Urology, Mohammed IV University Medical Center, Faculty of Medicine and Pharmacy, Mohammed the First University Oujda, Oujda, Morocco 
Received: 27 May 2020 - Accepted: 27 Jun 2020 - Published: 15 Jul 2020
Domain: Urology
Keywords: Emphysematous cystitis, bladder rupture, paraplegic, neurogenic bladder
©Abdelghani Ouraghi et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Abdelghani Ouraghi et al. Emphysematous cystitis complicated by bladder rupture: a paraplegic patient case. PAMJ Clinical Medicine. 2020;3:113. [doi: 10.11604/pamj-cm.2020.3.113.23778]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/113/full
Emphysematous cystitis complicated by bladder rupture: a paraplegic patient case
Abdelghani Ouraghi1,&, Amine El Houmaidi1, Arik Mhanna1, Mohamed Irzi1, Mehdi Chennouf1, Anouar El Moudane1, Ali Barki1
&Corresponding author
Most cases of bladder rupture are traumatic. Spontaneous rupture is more rare, especially the one due to emphysematous cystitis (EC) which has been reported in only nine cases in the literature. In our case, we report a 45 years old paraplegic patient with emphysematous cystitis and bladder rupture due to a urinary retention which causes him a urinary peritonitis treated with emergency laparotomy for repairing the wall of the bladder and antibiotics.
Emphysematous cystitis is extremely rare with less than 250 cases reported. Only nine cases of infectious rupture bladder described, it is an uncommon condition characterized by the presence of air within the bladder wall and lumen, it most commonly occurs in diabetic female patients or due to immunosuppression, recurrent urinary tract infections and neurogenic bladder or indewelling catheter. Case reports of emphysematous cystitis describe Escherichia coli as the most frequent causative pathogen. Other culprit organisms include Klebsiella pneumoniae, Enterobacter aerogenes, and Candida albicans. A delayed diagnosis can also result in bladder rupture, overwhelming infection and death [1, 2]. Our patient was an immunocompetent male, and also a paraplegic with a neurogenic bladder who had a bladder rupture due to EC.
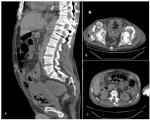
Our patient is a 45 year old, who had a long history of urinary tract infections, a paraplegia and undwelling foley catheter. He suffered for almost two days of severe pain, fever and acute urinary retention before he got brought to the Emergency Department of Mohammed VI Hospital in Oujda, Morocco. He was febrile to 39, tachycardic and hypotensive. Physical examination revealed a conscious patient with generalized abdominal tenderness and distended bladder with a non-functioning catheter. Laboratory data showed: white blood cells count at 30 K/ul, hemoglobin at 7.3 g/dL and C- reactive protein at 200 mg/dL, creatinine at 40 mg/l. Urinalysis revealed 11-70 WBC/HPF,> 80 RBC/HPF and positive nitrates. The puyria was managed with a dual-current probe ch 22 with a saline wash, and intravenous ceftriaxone and metronidazole. An abdominal computed tomography (CT) (Figure 1) scan was performed without contrast; it revealed the presence of a thickened bladder wall, with intramural gas bubbles and opacification of perivicular fat. The next day we found a blockage of the catheter. After an encouraging urinary flow, oliguria led us to suspect a rupture of the bladder that was confirmed by an urgent CT scan (Figure 1). In front of this urinary peritonitis, it was decided to do an exploratory laparotomy. At the opening of the peritoneum, there is a diffuse purulent effusion throughout the abdominal cavity (Figure 2). The bladder edges were debrided to healthy tissue, a suprapubic catheter and urethral catheter were placed, and the bladder was closed in two layers. Post-operatively the patient was transferred to the Intensive Care Unit (ICU) for sepsis management, and he died 2 days later.
Emphysematous cystitis (EC) is a distinct complicated lower urinary tract infections (UTI) characterized by air within the bladder wall and lumen. The disease is typically observed in elderly women (60-70 years of age) with severe diabetes mellitus, with cases reported approximately twice as often in women as in men. Traditional risk factors for UTIs, such as diabetes mellitus (DM), neurogenic bladder, recurrent urinary tract infections (UTI) and urinary stasis secondary to bladder outlet obstruction (BOO), are also risk factors for EC because it is considered to be a form of complicated UTI. Among the risk factors for EC, DM appears to be the strongest (70%) [1,2]. Among the microorganisms involved in this pathology, Escherichia coli (60%) and Klebsiella pneumoniae (10-20%). The EC can have a triad of pathogenic mechanisms including a metabolic factor (hyperglycemia, glucosuria and albuminuria), a bacteriological factor produced by the fermentation of glucose germs, which causes gas formation in the bladder wall. And an obstructive factor like a neurogenic bladder) [3]. Neurogenic bladder causes bladder ischemia which can be responsible for a mild inflammatory reaction and a lower antibiotic delivery, by decreasing the capillary blood flow to the infection site. It can result from two factors: bladder overdistention and increased intravesical pressure.
The clinical signs of EC are highly variable, ranging from asymptomatic to severe sepsis. The most common symptom is abdominal pain and Gross hematuria (60%). We can have other symptoms (ischuria, fever, pneumaturia and signs of acute cystitis). Performing urinalysis gram staining of the urine and the urine culture is essential for detecting the responsible pathogen. The CT plays an important role in the diagnosis of emphysematous cystitis. It shows the presence of air in the bladder wall which is characterized by a cobblestoned or “beaded necklace” appearance, reflecting irregular thickening of the non- dependent mucosal surface due to submucosal blebs. CT also reveals the severity of the condition (e.g, ascending emphysematous infections, intra-abdominal abscesses, adjacent neoplasic disease or bladder rupture just like our case) [4]. Concerning the treatement, approximately 90% of cases are treated with medical therapy alone, whereas 10% require combined surgical and medical intervention [5]. Medical therapy for complicated cystitis consists on parenteral antibiotics like fluoroquinolone, ceftriaxone, carbapenem and aminoglycoside [6]. Bladder drainage, by a Foley catheter enables the clinician to monitor the urinary status. In the presence of a significant amount of blood clots or difficulty voiding, bladder irrigation may be required to prevent bladder tamponade [5]. The treatment of predisposing conditions: controlling the glycemic level has been found to be successful in reported cases [7].
Surgery is required in patients exhibiting a poor response to initial medical management or those with severe necrotizing infections. In about 10% of cases, surgery is necessary and may consist of surgical debridement, partial cystectomy, total cystectomy or even nephrectomy in combined emphysematous cystitis/pyelonephritis emphysematous cases [8]. The paraplegic patient in the present case was diagnosed as having a bladder rupture as complication of emphysematous cystitis, after imaging investigation. And this complication is due to many risk factors such as neurogenic bladder which caused by his spinal cord injury (SCI). As SCI patients´ bladders have a no contractile ability, it may be subject to high intravesical pressure during filling. It can lead to reduced blood flow and vesicoureteral reflux which is a risk factor for UTI in neurogenic bladder that can leads to EC [9]. The emphysematous cystitis is almost certainly under-diagnosed as not all patients undergo radiological investigation especially the ones with no risk factors nor like our patient, who was a non-diabetic male and also with a poor sense of fullness of bladder, however it should be considered in order to minimize complications because a delay in diagnosis can lead in life threatening ones like in our case.
The diagnosis of bladder rupture due to EC can sometimes be difficult, especially in paraplegic patients who do not express the symptoms of pain. A high degree of suspicion in the management is therefore essential, especially in patients with a cause of urine retention. The use of imaging is necessary in these patients, especially CT, which remains the examination key to confirm the diagnosis and assessment of lesions, and to look for associated kidney lesions.
The authors declare no competing interests.
All authors contributed to the writing of this work. The authors have read and approved the final version of this work.
Figure 1: this axial and sagittal “non-contrast” abdominal CT scan shows: intra peritoneal effusion and free air, and air within the bladder wall (due to a bladder rupture complicated of urinary peritonitis
Figure 2: exploratory laparotomy: bladder rupture
- Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: a review of 135 cases. BJU Int. 2007;100(1):17-20. PubMed | Google Scholar
- Amano M, Shimizu T. Emphysematous cystitis: a review of the literature. Intern Med. 2014;53(2):79-82. PubMed | Google Scholar
- Banñón Pérez VJ, García Hernández JA, Valdelvira Nadal P, Nicolás Torralba JA, Server Pastor G, Coves R et al. Intraperitoneal bladder perforation in emphysematous cystitis. Actas Urol. 2000;24(6):501-503. Google Scholar
- Gheonea IA, Stoica Z, Bondari S. Emphysematous cystitis. Case report and imaging features. Curr Heal Sci J. 2012;38(4):191. PubMed
- Grupper M, Kravtsov A, Potasman I. Emphysematous cystitis: illustrative case report and review of the literature. Medicine (Baltimore). 2007;86(1):47-53. PubMed | Google Scholar
- The New England Journal of Medicine. Downloaded from nejm org at UAB Lister Hill Library on December 22, 2012 For personal use only No other uses without permission. Copyright © 1993 Massachusetts Medical Society All rights reserved. 1993.
- Yoshida K, Murao K, Fukuda N, Tamura Y, Ishida T. Emphysematous cystitis with diabetic neurogenic bladder. Intern Med. 2010;49(17):1879-1883. PubMed | Google Scholar
- Viswanathan S, Rajan RP, Iqba Nl, Subramani J, Report C. Enterococcus faecium related emphysematous cystitis and bladder rupture. Australas Med J. 2012; 5(11): 581-584. PubMed | Google Scholar
- Dinh A et al. Prise en charge des infections urinaires sur vessie neurologique. Med Mal Infect. 2019.