Abscess within a brain metastasis
Hassan Baallal, Fjouji Salah-Eddine, Badr Slioui, Ali Akhaddar
Corresponding author: Hassan Baallal, Department of Neurosurgery, Avicenne Military Teaching Hospital, University Caddi Ayyad, Marrakech, Morocco 
Received: 26 May 2020 - Accepted: 27 Jun 2020 - Published: 15 Jul 2020
Domain: Neuro-oncology,Surgical oncology
Keywords: Abscess, metastatic, cervical carcinoma
©Hassan Baallal et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Hassan Baallal et al. Abscess within a brain metastasis. PAMJ Clinical Medicine. 2020;3:115. [doi: 10.11604/pamj-cm.2020.3.115.23755]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/115/full
Abscess within a brain metastasis
Hassan Baallal1,2,&, Fjouji Salah-Eddine2, Badr Slioui1,2, Ali Akhaddar1
&Corresponding author
Detection of metastases especially intracranial metastases signals a poor prognosis in a patient with cancer. Solitary cystic metastasis is often difficult to differentiate from intra-cerebral abscess which can also occur in these patients. However, the co-existence of an abscess within a CNS metastasis is a rare event. At surgery, a purulent exudate within discrete metastatic tumours was identified. Pathological and microbiological examinations confirmed the coexistence of an abscess within a metastatic carcinoma. This case highlights the importance of considering intratumoral abscesses.
Brain metastasis from cervical cancer is a rare occurrence. With only approximately 100 cases of reported intracranial metastases of cervical cancer in the literature, proper management of these patients remains unclear [1]. However, cystic Brain metastases from carcinoma of the uterine cervix are uncommon and isolated necrotic metastases extremely rare. Although brain metastasis from ovarian/peritoneal cancer is rare, with an incidence of 0.3-5%, it usually results in dismal prognosis [2]. However, the co-existence of an abscess within a CNS metastasis is a rare event.We described a case of an abscess within isolated necrotic solitary metastasis of the brain from cervical cancer , and reviewed the literature to characterize more clearly the clinical presentation, treatment, and prognosis of patients with this condition.
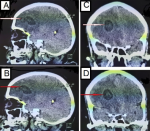
A 55-year-old right-handed woman She had entered menopause 8 years earlier presented.There was no significant past medical, in August 2019 to the emergency department with a 1-week history of progressive mild left-sided weakness and confusion. This was soon followed by difficulties in walking On the day of presentation, she developed a severe headache with vomiting, sudden-onset right-side hemiparesis and aphasia On examination in the emergency department she was confuse. She had a, left-sided sensory neglect, and a mild left hemiparesis. CT scan of her brain (Figure 1) showed a solitary 6 cm X 4 cm X 4 cm heterogeneous solid mass at the right fronto parietal junction with surrounding edema, mass effect. Nausea and vomiting had appeared in the last few hours. She had a sudden deterioration in level of consciousness together with anisocoria, and the Glasgow Coma Scale was 6/15. She was intubated. The appropriate decision to operate the patient in emergency was taken, she was admitted in the operating room at midnight and then underwent a right frontal craniotomy for resection of tumor using micro-dissection technique. At surgery, (Figure 2) a purulent exudate within discrete metastatic tumours was identified. with a pseudoplane all around, enabling a grosstotal resection. Pathological and microbiological examinations confirmed the coexistence of an abscess within a metastatic carcinoma from cervical cancer, Because microbiological tests including anaerobic cultures were positive, we commenced intravenous administration of broad-spectrum antibiotics. this is the first case for this type of surgery in this region of Dakhla-Oued Ed-Dahab in Morocan Sahara. Extubation was successfully performed after 48 hours, The patient was discharged from the intensive care unit after 6 days,under spontaneous breathing with perfect conscience and remained in the Neurosurgery ward. Then, the patient was discharged after a 20-day hospital stay. In postoperatively, she benefited a complementary whole-brain radiotherapy. At 6 months, following the treatment of brain metastasis, the patient is asymptomatic and free of disease.
Brain metastases occur in 10% to 30% of adults and in 6% to 10% of children. Autopsy studies reveal intracranial metastasis in approximately 25% of patients who die of cancer [3]. However, the co-existence of an abscess within a CNS metastasis is a rare event We report a rare case of abscess within a cerebellar metastasis. In our literature search of articles published in English since 1965 using tumour, metastasis and brain abscess as textwords, we have only 27 reported cases of a primary or secondary brain tumour coexisting with an abscess. Brain metastases from cervical cancer are extremely rare. However, an increase in the incidence of brain metastases from cervical cancer has been noted in recent years. Majority of the patients presented with other systemic metastatic disease along with the brain metastasis. Only a small fraction of patients presented with isolated brain metastasis in the absence of any systemic disease. Because of the rarity of brain metastasis from ovarian carcinoma, most reports include singular cases or series of patients in which patient accrual occurred over prolonged periods of time during which treatment approaches and modalities changed. This increase may be related to an improved treatment of the primary lesions and, thus, a better survival of these patients [4]. The pathophysiological processes underlying the coexisting abscess and metastasis were unknown in our patient. Possible explanations include a pure chance occurrence, hematogenous co-metastasis of tumour cells and bacteria from an infected lung neoplasm or secondary infection of a pre-existing cerebellar metastasis. The last explanation may be the most likely because necrotic tissue at the centre of a metastasis could become infected from septic hematogenous emboli.
Henriksen [5] first reported brain metastases from cervical carcinoma in an autopsy study, in 1949. Few reports have been published since then on this clinical entity. The incidence of brain metastases in this setting has been reported to be about 5% to 1.2% in various clinical studies [6,7]. Depending on the location of metastasis within the central nervous system (CNS), patients may present with a variety of signs and symptoms. The most common symptom at presentation is headache, occurring in 24% to 53% of patients. This is followed by altered mental status (24%-31%), focal weaknesses (16%-40%), seizures (15%), and ataxia (9%-20%) [8]. Most metastases are hypodense on noncontrast CT but may not be well visualized amidst the surrounding hypodense edema. The pattern of MRI signal intensity of different metastases is not usually helpful in providing a specific diagnosis, but a few general observations have been made. Most metastases demonstrate prolonged relaxation time (high T2 signal). Metastases may demonstrate cystic necrosis. The aim of surgery in treating brain metastasis is to lengthen the survival time of patients while improving neurological conditions and performance status [9]. Surgical planning commonly involves detailed preoperative structural and functional imaging. Utilization of intraoperative image guidance, microsurgical techniques, perioperative neurologic monitoring reduces possibility of surgery related mortality and morbidity. Brain metastases indicate poor prognosis, likely exclusion from clinical trials, and cause neurological deficits that impair patient´s lives in fundamental ways. Existing therapies are restricted to palliative radiation and neurological surgery, with limited chemotherapeutic options [10]. Unfortunately, the diagnosis of brain metastasis continues to portend a poor prognosis for the vast majority of patients. Although some young patients with single metastases and controlled systemic disease may achieve a good outcome, most patients have an expected survival measured in months. Available therapies include surgery, radiotherapy, and chemotherapy.
This case highlights the importance of considering the coexistence of two diseases prior to surgery. The pathophysiological processes underlying the coexisting abscess and metastasis were unknown in our patient. Preoperatively considering the possibility that a brain tumor and a brain abscess may coexist, when we encounter cases with imaging characteristics of both lesion types, may improve treatment outcomes.This case highlights the importance of considering intratumoral abscesses.
The authors declare no competing interest.
All the authors have read and agreed to the final manuscript.
Figure 1: CT scan of her brain in sagittal plane (A and B) showed a solitary 6 cm × 4 cm × 4 cm heterogeneous solid mass at the right fronto parietal junction. The coronal plane (C and D) showed surrounding edema,with mass effect
Figure 2: peroperative view showed a purulent exudate within discrete metastatic tumours was identified. with a pseudoplane all around, enabling a grosstotal resection
- Friedman M, Nissenbaum M, Lakier R, Browde S. Brain metastases in early cancer of the uterine cervix: a case report. S Afr Med J. 1983 Sep 24;64(13):498-9. PubMed
- Ratner ES, Toy E, O´Malley DM, McAlpine J, Rutherford TJ, Azodi M et al. Brain metastases in epithelial ovarian and primary peritoneal carcinoma. Int J Gynecol Cancer. 2009 Jul;19(5):856-9. PubMed | Google Scholar
- Johnson JD, Young B. Demographics of brain metastasis. Neurosurg Clin N Am. 1996 Jul;7(3):337-44. PubMed | Google Scholar
- Lefkowitz D, Asconape J, Biller J. Intracranial metastases from carcinoma of the cervix. South Med J. 1983 Apr;76(4):519-21. PubMed | Google Scholar
- Henriksen E. The lymphatic spread of carcinoma of the cervix and of the body of the uterus. Am J Obstet Gynecol. 1949 Nov;58(5):924-42. PubMed | Google Scholar
- Cormio G, Pellegrino A, Landoni F, Regallo M, Zanetta G, Colombo A et al. Brain metastases from cervical carcinoma. Tumori. 1996;82(4):394-6. PubMed | Google Scholar
- Saphner T, Gallion H, Nagell JR, Kryscio R, Patchell RA. Neurologic complications of cervical cancer. A review of 2261 cases. Cancer. 1989 Sep 1;64(5):1147-51. PubMed | Google Scholar
- Schellinger PD, Meinck HM, Thron A. Diagnostic accuracy of MRI compared to CCT in patients with brain metastases. J Neurooncol. 1999;44(3):275-81. PubMed | Google Scholar
- Narita Y, Shibui S. Strategy of surgery and radiation therapy for brain metastases. Int J Clin Oncol. 2009 Aug;14(4):275-80. PubMed | Google Scholar
- Hambrecht A, Jandial R, Neman J. Emerging role of brain metastases in the prognosis of breast cancer patients. Breast Cancer (Dove Med Press). 2011;3:79-91. PubMed | Google Scholar