Near fatal asthma in the emergency department: should intubate or not?
Hanen Ghazali, Maroua Mabrouk, Raja Fadhel, Ines Chermiti, Héla Chabbeh, Sami Souissi
Corresponding author: Hanen Ghazali, Emergency Department, Regional Hospital of Ben Arous, Ben Arous, Tunisia 
Received: 15 Apr 2020 - Accepted: 27 Jun 2020 - Published: 15 Jul 2020
Domain: Emergency medicine,Pulmonology,Urgent Care Medicine
Keywords: Near fatal asthma, intubation, mechanical ventilation, emergency department
©Hanen Ghazali et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Hanen Ghazali et al. Near fatal asthma in the emergency department: should intubate or not?. PAMJ Clinical Medicine. 2020;3:116. [doi: 10.11604/pamj-cm.2020.3.116.22872]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/116/full
Near fatal asthma in the emergency department: should intubate or not?
Hanen Ghazali1,&, Maroua Mabrouk1, Raja Fadhel1, Ines Chermiti1, Héla Chabbeh1, Sami Souissi1
&Corresponding author
Near-fatal asthma (NFA) is described as acute asthma associated with a respiratory arrest or arterial carbon dioxide tension greater than 50 mmHg, with or without altered consciousness, requiring mechanical ventilation. However, intubation and mechanical ventilation, in this category of asthmatic population, is a difficult managing task, especially in an emergency context. We reported the case of 23-year-old patient suffering from acute dyspnea presenting in our emergency department (ED) with a NFA associated to a respiratory peri arrest. Continuous nebulizers of bronchodilator therapy was successful with a good and rapid response to treatment. If intubation is an absolute indication for cardiac or respiratory arrest, it is based on clinical judgement and evolvement after aggressive and optimal therapy in NFA patients.
Near-fatal asthma (NFA) is described as acute asthma associated with a respiratory arrest or arterial carbon dioxide tension greater than 50 mmHg, with or without altered consciousness, requiring mechanical ventilation. However, intubation and mechanical ventilation, in this category of asthmatic population, is a challenging task which should be kept as a last resort. We herein present a case of a NFA managed successfully, with continuous nebulizers of bronchodilator therapy, in the emergency department (ED).
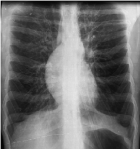
A 23-year-old male presented to the ED, by his own means, for acute onset dyspnea associated to an altered mental status. He had a history of previous severe asthma exacerbation three years ago leaded to intensive care unit (ICU) admission, and continuous history of smoking. The first assessment of vital signs showed a patient in peri respiratory arrest: obstructed-threatening airway, peripheral cyanosis, respiratory rate = 10 breaths/min, accessory muscles use, bilateral auscultator silence, pulse oximetry = 56% on air room, blood pressure= 150/100 mmHg, heart rate = 140bpm, no signs of peripheral hypo perfusion neither obstructive shock, GCS= 6/15, blood sugar rate= 2g/l. Ventilation was immediately supported by using bag mask device for five insufflations. Subsequent management included: continuous nebulizer bronchodilator therapy, which associated β2 agonists and anticholinergics agents on oxygen (6-8l/min) and systemic corticosteroid therapy (80 mg of methylprednisolone IV). As an adjunct to the first line therapy, he received a single dose of 2g Magnesium sulphate infusion and IV infusion of β2 agonists 0.5mg/h. Initial blood gas analysis showed respiratory acidosis with hyperlactatemia (ph=6.80, paCO2>115 mmHg, lac=7.7 mmol/l). Evolvement after 15 minutes of optimal and aggressive therapy: respiratory rate= 25 breaths/min, diminish use of accessory muscles, bilateral sibilant rattles, pulse oximetry= 100% on 8l/min oxygen, blood pressure= 120/70 mmHg, heart rate= 115bpm, and GCS= 15/15. Second blood gas analysis showed: ph=7.10, paCO2=76 mmHg, paO2=128 mmHg, lac=3.4 mmol/l, HCO3=23 mmol/l, SaO2=98%. Biological investigations showed leukocytosis 19940/mm3 (PNN=11930/mm3 and PNE=380/mm3). Chest radiography (Figure 1) showed signs of hyperinflation: heart in drop, linear ribs and narrow intercostal spaces. The patient was transferred to ICU within four hours and discharged to home at day seven with better control of his asthma.
In the USA, fewer than 10% of patients have exacerbations severe enough to be judged life threatening, whereas around 2-20% of patients are admitted to the ICU and 4% of patients are finally intubated and mechanically ventilated [1]. NFA has two distinctive phenotypes: the most common, responsible for 80-85% of all fatal events, is characterized by eosinophilic inflammation associated with gradual deterioration over days or weeks occurring in patients with severe and poorly controlled asthma and is slow to respond to therapy. The second phenotype, with neutrophilic inflammation, has both rapid onset and response to therapy [2].
Although cardiac or respiratory arrest represents an absolute indication for intubation, in NFA patients, the decision to intubate is essentially based on clinical judgement and should be considered for patients with progressive deterioration and/or poor response to aggressive treatment and not be embarked upon lightly.
The authors declare no competing interest.
All the authors have read and agreed to the final manuscript.
Figure 1: chest radiography performed after clinical stabilisation
- Papiris SA, Manali ED, Kolilekas L, Triantafillidou C, Tsangaris I. Acute Severe Asthma: New Approaches to Assessment and Treatment. Drugs. 2009;69(17):2363-91. PubMed | Google Scholar
- Holley AD, Boots RJ. Review article: management of acute severe and near-fatal asthma. Emerg Med Australas. 2009;21(4):259-68. PubMed | Google Scholar