Unusual ocular manifestation revealing Takayasu´s Arteritis
Amine Zahaf, Besma Ben Achour, Houda Lajmi, Mohammed Habib Lahdhiri, Wassim Hmaied
Corresponding author: Amine Zahaf, Department of Ophthalmology, Internal Security Forces Hospital, 29 Rue Tahar Ben Achour, 2078, La Marsa, Tunis, Tunisia 
Received: 30 May 2020 - Accepted: 27 Jun 2020 - Published: 16 Jul 2020
Domain: Internal medicine,Ophthalmology
Keywords: Takayasu´s arteritis, anterior ischemic optic neuropathy, Takayasu´s retinopathy
©Amine Zahaf et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Amine Zahaf et al. Unusual ocular manifestation revealing Takayasu´s Arteritis. PAMJ Clinical Medicine. 2020;3:117. [doi: 10.11604/pamj-cm.2020.3.117.23856]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/117/full
Unusual ocular manifestation revealing Takayasu´s Arteritis
Amine Zahaf1,2,&, Besma Ben Achour1,2, Houda Lajmi1,2, Mohammed Habib Lahdhiri1, Wassim Hmaied1,2
&Corresponding author
Takayasu´s arteritis is a rare inflammatory vascular disease affecting mostly the aorta and its proximal branches. The diagnosis of TA is a challenge, particularly in its initial phase. Here we report a case of a 20-years-old female presented with painless and sudden vision decrease in the left eye secondary to anterior ischemic optic neuropathy. After systemic examination and Magnetic Resonance Angiography of vessels, the diagnosis of Takayasu´s arteritis was made. She was treated with steroids, Azathioprine, and Tocilizumab. At 3 months of follow-up, there was no improvement in the visual acuity of the left eye and fundus examination showed atrophy of the left optic disc.
Takayasu´s arteritis (TA) is a rare chronic inflammatory disease of unknown origin, involving the aorta and its branches leading to narrowing and obliteration. Ocular manifestations are common in TA. Nevertheless, anterior ischemic optic neuropathy (AION) has been rarely reported. Here we report a case of a young female presenting unilateral AION as the initial manifestation of TA.
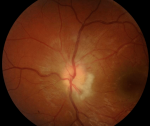
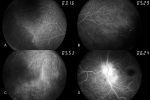
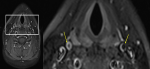
A 20-year-old female presented with a painless and sudden vision decrease in the left eye (OS). On ocular examination, she had best-corrected visual acuity of 10/10 in the right eye (OD) and 1/10 in the OS. A relative afferent pupillary defect was noted in the OS, while slit-lamp examination and tonometry were normal in both eyes. The funduscopic evaluation revealed optic disk edema, peripapillary cotton wool spots, and multiple retinal micro-aneurysms in peripheral retina in the OS while the OD was normal (Figure 1). Fundus fluorescein angiography (FFA) revealed in the OS a delayed arm to retina time, microaneurysms, telangiectasia, extensive area of peripheral capillary nonperfusion, and fluorescein leakage in the optic disk in the late stage (Figure 2). In the OD, FFA revealed some areas of peripheral capillary non-perfusion. Systemic examination showed a 20-mm Hg difference in blood pressure between arms and vascular bruits in the right carotid and subclavian arteries. Results of the erythrocyte sedimentation rate and C reactive protein were normal. Magnetic Resonance Angiography of vessels showed regular, diffuse, and circumferential thickening of the two carotid arteries, a very tight post bulbar stenosis of the two internal carotid arteries, a left ophthalmic artery hypertrophic, and narrowness of the right ophthalmic artery (Figure 3). The diagnosis of TA was made after satisfying four of the six criteria described by the American College of Rheumatology. She was treated with steroids (intravenous Methylprednisolone 1000 mg/day for 3 days followed by a course of oral steroids), Azathioprine (150mg/day), and intravenous Tocilizumab (480mg). Cardiovascular surgeons did not indicate surgery or endovascular revascularization. We realized photocoagulation of the area of capillary nonperfusion in the OS. At 3 months of follow-up, there was no improvement in the visual acuity of the OS and fundus examination showed atrophy of the left optic disc.
Takayasu´s arteritis is an inflammatory vascular disease affecting more females than males. It usually begins in the second or third decade of life and involves primarily the large arteries. It was first reported in 1908 by Takayasu, a Japanese ophthalmologist [1]. While the disease has a worldwide distribution, Asian populations are generally the most affected [2]. The diagnosis of TA is a challenge, particularly in its initial phase. In fact, systemic symptoms occurred in only a third of patients, erythrocyte sedimentation rate lack sensitivity, and there is no diagnostic serologic test [3]. According to The The American College of Rheumatology [4], three of the following criteria are mandatory to retain the diagnosis of TA: onset before 40 years, decrease in the brachial pulse in one or both arms, claudication of the extremities, audible bruit on auscultation of the aorta or subclavian artery difference of 10 mm Hg or more in blood pressure measured in both arms, narrowing at the aorta or its primary branches on arteriogram. Ocular changes in TA were the consequence of the progressive narrowing of major vessels of the neck and resultant ocular hypoperfusion. The most frequent manifestation was Takayasu´s retinopathy which had been classified into four stages by Uyama and Asayma [5]. Our patient presented an extensive area of retinal ischemia in the OS and was classified in the fourth stage. Other ischemic manifestations have been infrequently described like central retinal artery occlusion, ocular ischemic syndrome, and AION [6-8]. the rarity of ischemic optic neuropathy in young patients suffering from TA might suggest a protective role of the peripapillary capillary changes, which are a hallmark of the disease [6]. Treatment of TA is based on the use of anti-inflammatory therapy like steroids and/or methotrexate to decrease or to stop the inflammatory activity. Recently, Tocilizumab, an interleukin-6 receptor monoclonal antibody, has proven its effectiveness in the treatment of TA and may reduce the incidence of relapses [9]. Both surgical and endovascular treatments may be risky and achieve poorer outcomes if they are undertaken during the period of inflammatory activity [10].
AION may represent the inaugural sign of systemic disease in young patients such as TA. We reported a rare case presenting with acute visual loss secondary to AION, without other systemic symptoms, revealing TA. Our case highlights the necessity of systemic investigations to make rapidly the diagnosis. Multidisciplinary management is mandatory for a favorable outcome.
The authors declare no competing interests.
All authors have read and agreed to the final version of this manuscript and have equally contributed to its content and the management of the case.
Figure 1: fundus photograph of the left eye. optic disk edema and peripapillary cotton wool spots
Figure 2: fundus fluorescein angiography of the left eye. Nonperfused areas (A); arteriovenous shunts (B); telangiectasia of the peripheral retinal vessels (C); fluorescein leakage in the optic disk in the late-stage (D)
Figure 3: magnetic resonance angiography of vessels (T1 fat-saturation sequence). Regular, diffuse, and circumferential thickening of the two carotid arteries
- Takayasu S. A case with curious change in the central retinal artery. Nippon Ganka Gakkai Zasshi. 1908;12:554-5. Google Scholar
- Onen F, Akkoc N. Epidemiology of Takayasu arteritis. La Presse Médicale. 2017 Jul-Aug;46(7-8 Pt 2):e197-e203. PubMed | Google Scholar
- Kerr GS. Takayasu Arteritis. Ann Intern Med. 1994 Jun 1;120(11):919-29. PubMed | Google Scholar
- Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM et al. The American College of Rheumatology 1990 criteria for the classification of takayasu arteritis. Arthritis Rheum. 1990 Aug;33(8):1129-34. PubMed | Google Scholar
- Uyama M, Asayama K. Retinal Vascular Changes in Takayasu´s Disease (Pulseless Disease), Occurrence and Evolution of the Lesion, In: De Laey JJ, editor, International Symposium on Fluorescein Angiography Ghent 28 March-1 April 1976, vol 9. Dordrecht: Springer Netherlands. 1976;549-54. Google Scholar
- Karam EZ, Muci-Mendoza R, Hedges III TR. Retinal findings in Takayasu´s arteritis. Acta Ophthalmol Scand. 1999 Apr;77(2):209-13. PubMed | Google Scholar
- Tian G, Chen Q, Wang W. Takayasu arteritis presenting as isolated anterior ischemic optic neuropathy. Int Ophthalmol. 2018 Apr;38(2):823-828. PubMed | Google Scholar
- Hata M, Miyamoto K, Oishi A, Yoshimura N. Case of simultaneous bilateral anterior ischemic optic neuropathy associated with Takayasu disease. Canadian Journal of Ophthalmology. 2013 Apr;48(2):e33-5. PubMed | Google Scholar
- Mekinian A, Resche-Rigon M, Comarmond C, Soriano A, Constans J, Alric L et al. Efficacy of tocilizumab in Takayasu arteritis: Multicenter retrospective study of 46 patients. Journal of Autoimmunity. 2018 Jul;91:55-60.. PubMed | Google Scholar
- Tyagi S, Sharma VP, Arora R. Stenting of the Aorta for Recurrent, Long Stenosis Due to Takayasu´s Arteritis in a Child. Pediatr Cardiol. 1999;20(3):215-7. PubMed | Google Scholar