Wernicke´s encephalopathy in hyperemesis gravidarum: rare case report
Soukaina Wakrim
Corresponding author: Soukaina Wakrim, Service de Radiologie, Faculté de Médecine et de Pharmacie, Université Ibn Zohr, Agadir, Maroc 
Received: 10 Apr 2020 - Accepted: 18 May 2020 - Published: 08 Jun 2020
Domain: Neurology (general),Obstetrics and gynecology
Keywords: Encephalopathy of Wernicke, diagnosis, magnetic resonance imaging (MRI)
©Soukaina Wakrim et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Soukaina Wakrim et al. Wernicke´s encephalopathy in hyperemesis gravidarum: rare case report. PAMJ Clinical Medicine. 2020;3:42. [doi: 10.11604/pamj-cm.2020.3.42.22771]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/42/full
Wernicke's encephalopathy in hyperemesis gravidarum: rare case report
Soukaina Wakrim1,&
1Service de Radiologie, Faculté de Médecine et de Pharmacie, Université Ibn Zohr, Agadir, Maroc
&Corresponding author
Soukaina Wakrim, Service de Radiologie, Faculté de Médecine et de Pharmacie, Université Ibn Zohr, Agadir, Maroc
Wernicke´s encephalopathy is a neurological emergency secondary to thiamine deficiency (vitamin B1). It is most frequently found in alcoholics, severe malnutrition and gastric cancers. It associates the triad (confusion, ataxia, ophthalmoplegia). Cerebral MRI is the first-line radiological examination. The encephalopathy of Wernicke in pregnancy is an unknown pathology, poor prognosis, which occurs secondarily to hypermesis gravidarum. The prevention of Wernicke´s encephalopathy requires obligatory management of hyperemesis gravidarum, including the preventive administration of thiamine. This work aims to analyze the diagnostic management of pregnant woman with encephalopathy Wernicke. Our work is the case report of a woman the 25-year-old who presented serious impairment of consciousness. The gestational age at the time of the manifestations was 12 weeks. MRI brain is performed and found classic signs of encephalopathy Wernicke.
Wernicke´s encephalopathy (WE) is a syndrome neuropsychiatric due to thiamine deficiency, potentially fatal but not fatal avoidable, there are multiple risk factors. The clinical presentation is extremely varied with the presence of the triad typical clinic for most cases (confusion, ataxia, ophthalmoplegia). However, it may be incomplete or associated with other clinical signs (convulsion, dysarthria). On MRI, there are hyper signals from the affected areas in sequence T2, FLAIRE, and in diffusion. Therapeutic management consists of the administration of thiamine as soon as possible before glucose administration to avoid sequelae irreversible neurological damage.
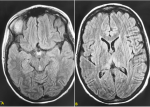
We present the case the woman of 25-year-old with no particular medical or obstetrical personal history was pregnant with a second pregnancy, which was not followed up medically. The history of her illness had begun around 10 weeks of amenorrhea (AS), where she began to develop vomiting of moderate abundance at first and whose daily frequency increased along the pregnancy, as well as the volume that was becoming more and more abundant. These vomiting were accompanied by epigastric abdominal pain and weight loss depending on the parturient, but which remains unquantified. Then the patient presented serious impairment of consciousness, ophthalmoplegia, nystagmus and ataxia why she hospitalized in the intensive care unit. She had hydroelectrolytic disorders: hypokalemia, hypochloremia and hyponatremia associated with liver damage (cytolysis and hepatic cholestasis) and a renal failure (creatinemia at 24 mg/l, and urea at 2.05 g/l). According to Caine's criteria [1], the clinical and biological picture was in favor of hyperemesis gravidarum with severe hydroelectrolytic disorders. Magnetic resonance imaging was performed using 1.5-T MRI with sagittal T1-weighted, transverse T2-weighted, and transverse FLAIR and Diffusion. The cerebral MRI objectived in FLAIR and diffusion sequence a hyper signal at the internal part of the two thalami and at the level of the mammary bodies (Figure 1), characteristic of Wernicke´s encephalopathy. The patient received thiamine with an emergency dose of 300 mg for 3 times daily intravenously. Then a dose of 6OO mg/day, in the state phase. She had sequelae in the form of tetraparasia. The fetal prognosis is favorable.
Wernicke´s encephalopathy (GWE) is a syndrome neuropsychiatric due to a potentially fatal but preventable thiamine deficiency, characterized by the classic triad of encephalopathy, ophthalmoplegia, ataxia, and mental confusion [2]. At the physiological level, thiamine is a water-soluble essential vitamin. The daily requirement is 5 mg and is usually provided by diet. The body stock is about 25 to 30 mg. Thiamine is an essential cofactor of 3 enzymes involved in energy metabolism, in glucose degradation [3-5]. EW is mainly observed in alcoholics, but can also appear in any state of malnutrition. In obstetrics, hyperemesis gravidarum can be complicated by EW due to low thiamine reserves, as well as increased needs [6]. Nowadays, there is no consensus on early diagnosis, treatment and the prevention of this disorder. A series of papers nowadays emphasize diagnostic the ocular motor signs in pre-encephalopathy patients with nutritional deficiency at risk of thiamine deficiency and timely recognition of thiamine depletion in these patients, who may have a normal brain MRI, could lead to appropriate management and prevention of Wernicke´s encephalopathy (WE) with full recovery. The second aim is to incorporate recent diagnostic testing on the revised WE diagnostic criteria and the identification of patients who may show slow, partial, or no response to treatment [7].
Imaging studies have been extensively used in the evaluation of WE to improve diagnostic accuracy. Computed tomography (CT) is well suited to demonstrate only the hemorrhagic lesions [8,9]. A review of the literature on contrast-enhanced CT in the acute phase of WE demonstrated nonuniform results, and furthermore, Antunez et al. [10] demonstrated a very low sensitivity (13.3%) of CT for the diagnosis of WE. On the contrary, magnetic resonance imaging (MRI) yields high diagnostic sensitivity allowing identification of typical signs of WE, including symmetrically increased signal intensity in the mesencephalic tegmentum, mammillary bodies, and medial thalamus depicted on T2-weighted and FLAIR sequences [11]. Victor and all in the Wernicke-Korsakoff Syndrome book, were that this remains, and will remain, the definitive work on the effects of alcohol and malnutrition on the human nervous system. The original descriptions by Wernicke and Korsakoff are reviewed and a very detailed account of the clinical phenomena is presented based on the original study of 245 patients and autopsy examinations of 82 of these [12]. Any pregnant woman with hyperemesis gravidarum or a state of malnutrition should be supplemented daily with thiamine. The functional prognosis is poor if care is delayed. A better knowledge of the entire pathology and a better understanding of the disease raising awareness among medical staff would improve prognosis [13,14]. Depending on the time before the start of treatment, the evolution can go from complete reversibility disorders, motor sequelae, Alzheimer's syndrome, and Korsakoff, in a coma, even death [15].
The encephalopathy of Wernicke is a rare pathology during pregnancy. It must be suspected before any neurological disorder occurring in a context of precarious nutritional status, especially in the case of hyperemesis gravidarum. Early treatment with vitamin supplementation (thiamine) makes it possible to have a favorable evolution and to avoid the persistence of the neurological disorders. In case of delayed diagnosis or treatment, the neurological sequelae can be definitive until death.
The authors declare no competing interest.
All the authors have read and agreed to the final manuscript.
Figure 1: (A,B) MRI in transverse FLAIR objectified a hypersignal in FLAIR of the internal parts of the thalamus on either side of the V3 as well as of the mamillary bodies
- Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: identification of Wernicke's encephalopathy. J Neurol Neurosurg Psychiatry. 1997 Jan;62(1):51-60. PubMed | Google Scholar
- Einarson TR, Piwko C, Koren G. Quantifying the global rates of nausea and vomiting of preg- nancy: a meta-analysis. J Popul Ther Clin Phar- macol. 2013;20(2):e171-83. PubMed | Google Scholar
- Al-Yatama M, Diejomaoh M, Nandakumaran M, Monem RA, Omu AE, Al Kandari F. Hormone profile of Kuwaiti women with hyperemesis gravidarum. Arch Gynecol Obstet. 2002 Aug;266(4):218-22. PubMed | Google Scholar
- Phayphet M, Rafat R, Andreux F, Parraga E, Rondeau E, Hertig A. Hyperemesis gravidarum: une cause rare de l´encépahalopathie de wernicke. Presse Med. 2007 Dec;36(12 Pt 1):1759-61. PubMed | Google Scholar
- Eboué C, Carlier-Guérin C, de La Sayette V, Grall JY, Herlicoviez M. Une complication rare des vomissements gravidiques: l´encéphalopathie de GayetWernicke. J Gynecol Obstet Biol Reprod (Paris). 2006;35(8):822-5. Google Scholar
- Hastoy A, Lien Tran P, Lakestani O, Barau G, Gérardin P, Boukerrou M. L'hyperémèse gravidique : quelles conséquences sur la grossesse. J Gynecol Obstet Biol Reprod. 2015;44(2):154-63. Google Scholar
- Kattah JC. The Spectrum of Ocular Motor and Vestibular abnormalities in Thiamine Deficiency. Curr Neurol Neurosci Rep. 2017 May; 17(5):40. PubMed | Google Scholar
- Spruill SC, Kuller JA. Hyperemesis gravidarum complicated by Wernicke´s encephalopathy. Obstetrics and Gynecology. 2002 May;99(5 Pt 2):875-7. PubMed | Google Scholar
- Manzo G, De Gennaro A, Cozzolino A, Serino A, Fenza G, Manto A. MR in alcoholic and nonalcoholic acute Wernicke's encephalopathy: a review. Biomed Res Int. 2014;2014:503596. PubMed | Google Scholar
- Antunez E, Estruch R, Cardenal C, Nicolas JM, Fernandez-Sola J, Urbano-Marquez A. Usefulness of CT and MR imaging in the diagnosis of acute Wernicke´s encephalopathy. AJR Am J Roentgenol. 1998 Oct;171(4):1131-7. PubMed | Google Scholar
- Zuccoli G, Pipitone N. Neuroimaging findings in acute Wernicke's encephalopathy: review of the literature. AJR Am J Roentgenol. 2009 Feb;192(2):501-8. PubMed | Google Scholar
- Victor M, Adams RD, Collins GH. The Wernicke-Korsakoff Syndrome and Related Neurologic Disorders due to Alcoholism and Malnutrition. Contemporary Neurology Series 30. 1989. Google Scholar
- Sriram K1, Manzanares W, Joseph K. Thiamine in nutrition therapy. Nutr Clin Pract. 2012 Feb;27(1):41-50. Google Scholar
- Sechi G, Serra A. Wernicke´s encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol. 2007 May;6(5):442-55. PubMed | Google Scholar
- Chiossi G, Neri I, Cavazzuti M, Basso G, Facchinetti F. Hyperemesis gravidarum complicated by Wernicke encephalopathy: Background, case report, and review of the literature. Obstet Gynecol Surv. 2006;61(4):255-268. PubMed | Google Scholar