Monstrous glomus tumor of nail bed clinical and dermoscopic appearance: case report
Jihane Ziani, Fatima Zahra Mernissi, Salim Gallouj
Corresponding author: Jihane Ziani, Department of Dermatology, Hassan II University Hospital, Fez, Morocco 
Received: 05 May 2020 - Accepted: 30 May 2020 - Published: 18 Jun 2020
Domain: Dermatology
Keywords: Dermoscopy; Glomus tumor; Nail bed lesion.
©Jihane Ziani et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Jihane Ziani et al. Monstrous glomus tumor of nail bed clinical and dermoscopic appearance: case report. PAMJ Clinical Medicine. 2020;3:60. [doi: 10.11604/pamj-cm.2020.3.60.22396]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/60/full
Monstrous glomus tumor of nail bed clinical and dermoscopic appearance: case report
Jihane Ziani1,&, Fatima Zahra Mernissi1, Salim Gallouj2
&Corresponding author
The glomus tumor is a benign tumor with a low incidence compared to other degenerative tumors. They are to the detriment of the glomic body, a thermoregulatory device for cutaneous microvascularization. The diagnosis is often late, scented for years, which leads to significant morbidity in patients. We report the case of a 53-year-old woman with one year of pain in her right middle finger, who was diagnosed as a glomus tumor, with clinical and dermoscopic description, and who was surgically removed with the completion of a dermoscopy of the piece of excision and of the histopathological result compatible with a glomus tumor. The patient was relieved of functional signs immediately after surgery and the evolution noted no deformation of the affected nail without recurrence of symptoms with a follow-up of 3 years. Glomus tumors of the hand are a rare entity and the dermoscopic description of the tumor is poorly reported.
The glomus tumor is a rare and it´s a vascular benign tumor which comes from the neuromyoarterial cells of the normal glomus apparatus of the reticular dermis [1] supposed to function in thermal regulation. It represents approximately 1 to 4% of hand tumors [2]. The average age of onset of the tumor is between 30 and 50 years, but can occur at any age, as well as the average between the onset of symptoms and the exact diagnosis is around seven years [3].
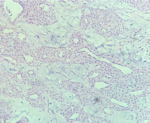
A 53-year-old woman came for consultation, with a cholecystectomized history 23 days ago, and pain at the end of the right middle finger for 6 months, no history of trauma preceding the lesion was reported with worsening of pain during exposure to cold and microtrauma. The development of his onychopathy was marked by changes in his nail in color and shape, with clinical examination, a monodigital pseudo-hypocratism of the nail of the right middle finger with an anterior incarnation, anterior onycholysis in V shape with chloronychia, and a visible erytronichic band (Figure 1). On dermoscopic examination, we noted an effacement of the lunula, a better visualization of onycholysis in V shape with the perception of a tree trunk at the level of the erytronichic band (Figure 2). X-ray of the hand did objectify a well limited tissue lesion on the dorsal side of the last phalanx of the 3rd right finger with bone deformation without osteolysis (Figure 3). The patient benefited from a surgical excision of the tumor, the intraoperative dermoscopy of the nail bed before delivery of the tumor to detect a purple red area with the presence of regular linear vessels (Figure 4). Thereafter we carried out an enucleation of the tumor and surgery to reduce the anterior edge using the Dubois technique. The anatomopathological result revealed a tumor proliferation arranged around numerous vascular slots circumscribed by regular flattened endothelial cells. These vessels, with sometimes thickened walls, are surrounded by several superimposed layers of ovoid cells with regular round glands and a scant and eosinophilic cytoplasm. (Figure 5). The evolution was marked by a normal growth of the nail 3 years back without abnormality of the nail plate or report of functional signs (Figure 6).
The pathological characteristics of glomus tumors were first described by Masson in 1924, they are mainly caused by hyperplasia of the glomus body and are located in the reticular dermis layer [4]. The etiology of glomus tumors is unknown and may be linked to sex, age, trauma or inheritance, they are mainly observed in women between 30 and 50 years old, with sizes generally less than 1 cm and are generally located at the extremities, with clinical features include a classic triad of excruciating pain, localized sensitivity and sensitivity to cold [5]. There are several differential diagnoses. The neuroma gives comparable pain and a trigger zone, but without hypersensitivity to cold and without vascular signs on arteriography or MRI. Melanoma is painless but may be visible under the nail. The fibrokeratoma and mucoid cyst are not very painful. The exostosis is visible on the radiography without preparation of the phalangette. The osteoid osteoma is also painful, the radiography suggestive with an intraosseous lacuna sometimes calcified, surrounded by an extended sclerosis. The hematoma is also painful, visible under the nail, within the framework of a small trauma of the finger, and the evolution is favorable in a few days, unlike the glomus tumor whose semiology is persistent. Radiography can show cortical thinning or erosive changes in the bone adjacent to the tumor [6]. Imaging such as Doppler ultrasound and MRI can help the diagnosis to exclude or reverse visualize and diagnose clinically normal glomus tumors, and therefore the interest of imaging is especially in subclinical cases and in cases of recurrence [7]. Ultrasound can in turn demonstrate the size, site and shape of the tumor, but it is a dependent operator [6,8]. The signs on MRI sought are a weak signal intensity on T1-weighted images, hyperintensity on T2-weighted images and an improvement on T1-weighted images after gadolinium injection [9].
To our knowledge, the dermoscopic description of glomus tumors, especially in gesture, is rarely reported in the literature. Dermoscopy of the nail plate can find the presence of linear vascular structures; however, these structures can often be discreet or absent. To better facilitate the diagnosis, we suggest the performance of the nail dermoscopy, and this before the tumor excision [10]. This procedure is performed during the intra-surgical period, when the nail bed is exposed after an anesthetic block and careful avulsion of the nail plate. Dermoscopic examination of the entire bed makes it possible to visualize the location of the tumor, its purple color and the visualization of the vascular pattern of the lesion, further suggesting the diagnosis of glomus tumor. Especially when the tumor is not encapsulated, the use of dermoscopy facilitates the delimitation of surgical margins during the intra-surgical period. It also allows, after excision of the lesions, the visualization of other residual macroscopic tumor foci in the nail machine. Something that can confuse other nail tumors and make the diagnosis difficult, therefore the key thing in the diagnosis is the patient's story of extreme pain on the local pressure on the nail fold and extreme local pain in cold weather and surgical excision is the only therapeutic option for immediate pain relief. Complete surgical excision is the only effective way to heal the glomus tumor. The proximal phalanx must be completely bloodless by a tourniquet and an additional second on the upper limb can be chosen in the event of a bad bloodless effect. There are two major surgical approaches to excise a subungual glomus tumor. The traditional approach is transungual excision, which removes part or all of the nail plate, and cuts through the nail bed to ensure good tumor exposure. Complete removal is relatively easy, but damage to the nail bed is obviously more severe, with a higher incidence of postoperative nail deformation. The other commonly used approach is the one we have. adopt for the care of our patient where the incision is lateral, L-shaped along the edge of the nail, and raises the nail plate to expose the nail bed and then the tumor. This approach leaves less damage and preserves the entire nail bed, reducing the risk of postoperative nail deformation.
Thanks to dermoscopy, the study of the nail bed reveals particular aspects which can only be observed when the nail plate is no longer interposed between the bed and the dermatoscope. It is a simple and inexpensive procedure, which does not replace histopathological examination, but which helps in the diagnosis and elimination of lesions and which does not entail additional risks for the patient who will undergo an intervention surgical.
The authors declare no competing interests.
All the authors have read and agreed to the final manuscript.
Figure 1: (A,B) clinical image. Monodigital pseudo-hypocratism of the nail of the right middle finger with an anterior incarnation
Figure 2: dermoscopic aspect of a glomus-cell tumor
Figure 3: (A,B) X-ray showing the scalloping of the opposite bone
Figure 4: (A) making a lateral avulsion; (B) dermoscopy, regular linear vascular pattern on an erythematato-purple background; (C) elevation of the proximal fold with a longitudinal incision of the nail bed; (D) tumor extraction; (E) dermoscopy, dome appearance with telangiectasia; (F) dubois technique
Figure 5: histological image.
Figure 6: (A,B) follow up after 3 years
- Chou T, Pan SC, Shieh SJ, Lee JW, Chiu HY, Ho CL. Glomus tumor: twenty-year experience and literature review. Ann Plast Surg. 2016;76(Suppl 1):S35-40. PubMed | Google Scholar
- Mitchell A, Spinner RJ, Ribeiro A, Mafra M, Mouzinho MM, Scheithauer BW. Glomus tumor of digital nerve: case report. J Hand Surg Am. 2012;37(6):1180-3. PubMed | Google Scholar
- David H Kim. Glomus Tumor of the Finger Tip and MRI Appearance. Iowa Orthop J. 1999;19:136-8. PubMed | Google Scholar
- Masson P. Le glomus neuromyo-arteriel des regions tactiles et ses tumeurs. Lyon Chi. 1924;21:257-280. Google Scholar
- Chen KB, Chen L. Glomus tumor in the stomach: a case report and review of the litera- ture. Oncol Lett. 2014 Jun;7(6):1790-1792. PubMed | Google Scholar
- Mitchell A, Spinner RJ, Ribeiro A, Mafra M, Mouzinho MM, Scheithauer BW. Glomus tumor of digital nerve: case report. J Hand Surg Am. 2012;37(6):1180-3. PubMed | Google Scholar
- Rosner IA, Argenta AE, Washington KM. Unusual volar pulp location of glomus tumor. Plast Reconstr Surg Glob Open. 2017;5(1):e1215. PubMed | Google Scholar
- Kim SW, Jung SN. Glomus tumour within digital nerve: a case report. J Plast Reconstr Aesthet Surg. 2011;64(7):958-60. PubMed | Google Scholar
- Chou T, Pan SC, Shieh SJ, Lee JW, Chiu HY, Ho CL. Glomus tumor : twenty-year experience and literature review. Ann Plast Surg. 2016;76(Suppl 1):S35-40. PubMed | Google Scholar
- Hirata SH, Yamada S, Almeida FA, Enokihara MY, Rosa IP, Enokihara MM et al. Dermoscopic examination of the nail bed and matrix. Int J Dermatol. 2006 Jan;45(1):28-30. PubMed | Google Scholar
Search
This article authors
On Pubmed
On Google Scholar
Citation [Download]
Navigate this article
Similar articles in
Key words
Tables and figures
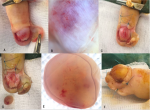 Figure 4: (A) making a lateral avulsion; (B) dermoscopy, regular linear vascular pattern on an erythematato-purple background; (C) elevation of the proximal fold with a longitudinal incision of the nail bed; (D) tumor extraction; (E) dermoscopy, dome appearance with telangiectasia; (F) dubois technique
Figure 4: (A) making a lateral avulsion; (B) dermoscopy, regular linear vascular pattern on an erythematato-purple background; (C) elevation of the proximal fold with a longitudinal incision of the nail bed; (D) tumor extraction; (E) dermoscopy, dome appearance with telangiectasia; (F) dubois technique