Spontaneous heterotopic pregnancy associated with the threat of abortion: diagnostic difficulties
Jihad Jamor, Alpha Boubacar Conte, Hikmat Chaara, Fatima Zohra Fdili Alaoui, Sofia Jayi, Moulay Abdelilah Melhouf
Corresponding author: Alpha Boubacar Conte, Department of Gynecology, Obstetrics II, Hassan II Teaching Hospital of Fez, Fez, Morocco 
Received: 16 Mar 2020 - Accepted: 18 May 2020 - Published: 25 Jun 2020
Domain: Obstetrics and gynecology
Keywords: Heterotopic pregnancy, trophoblastic detachment, threat of abortion, pelvic MRI
©Jihad Jamor et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Jihad Jamor et al. Spontaneous heterotopic pregnancy associated with the threat of abortion: diagnostic difficulties. PAMJ Clinical Medicine. 2020;3:73. [doi: 10.11604/pamj-cm.2020.3.73.22367]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/3/73/full
Case report 
Spontaneous heterotopic pregnancy associated with the threat of abortion: diagnostic difficulties
Spontaneous heterotopic pregnancy associated with the threat of abortion: diagnostic difficulties
Jihad Jamor1, Alpha Boubacar Conte1,&, Hikmat Chaara1, Fatima Zohra Fdili Alaoui1, Sofia Jayi1, Moulay Abdelilah Melhouf1
&Corresponding author
Defined as the association of intrauterine and ectopic pregnancies in an individual, spontaneous heterotopic pregnancy occurred rarely with an incidence of 1/30,000. We report a case of a spontaneous heterotopic pregnancy associating a ruptured right ampullar pregnancy with a progressive intra uterine pregnancy and trophoblastic detachment managed in our department of Gynecology-Obstetrics II of the Hassan II Teaching Hospital of Fez.
Heterotopic pregnancy is defined as the presence of intrauterine and ectopic pregnancies in an individual [1]. It is a rare form of twin pregnancy which was first described in 1708. With the advent of assisted medical procreation, the overall incidence of heterotopic pregnancy, which is reported at 1/30000 in spontaneous pregnancies has increased considerably and is estimated from 1.5 per 1000 to 1 per cent in assisted pregnancies [2,3]. Its diagnosis is not easy. Management is often difficult because the goal is to terminate the ectopic pregnancy by taking precautions to minimize the possible threat to intrauterine pregnancy [4]. We report a case of a spontaneous heterotopic pregnancy associating a ruptured right ampullar pregnancy with a progressive intrauterine pregnancy and trophoblastic detachment.
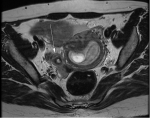
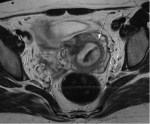
A 33-year-old patient, with no specific history and no known risk factors for ectopic pregnancy, G3P2 who consulted for the management of bleeding on an amenorrhea of 6 weeks and 2 days without any notion of induction of pregnancy in whom the examination found a patient hemodynamically and respiratory stable. The gynecological examination found on the abdominal palpation a flexible abdomen without contracture or defense, in the speculum a minimal bleeding coming from the endocervix with vaginal touching a right lateral uterine tenderness without palpable mass and a rectal examination without signs of peritoneal irritation. Pelvic ultrasound reveals the presence of an intrauterine gestational sac with yolk sac, embryonic sketches and positive cardiac activity associating a 19/33mm trophoblastic detachment and presence in right lateral uterus of a heterogeneous image of 52/38mm including nature is difficult to appreciate. We decided to complete the paraclinical assessment with a pelvic MRI which described a heterotopic pregnancy in which the active intrauterine one associates a significant trophoblastic detachment and that ectopic is ampullar with right tube seat of a hematosalpinx with heterogeneous thickening making 39 x 10mm in favor of an ectopic pregnancy (Figure 1, Figure 2). The patient underwent a right laparoscopic salpingectomy for the management of ectopic pregnancy after placement of 200μg of progesterone ovum into the posterior vaginal sac. During laparoscopy, the exploration found a hemoperitoneum of low abundance aspirated estimated at 100cc with an enlarged uterus corresponding to gestational age of 09 SA; in the left appendices the trunk was without particularity the ovary was the seat of a yellow body. In the right appendices, the ovary was macroscopically normal in appearance and the fallopian tube was the site of a ruptured ampullary pregnancy measuring 5/6 cm with the presence of trophoblastic tissue at the level of the Douglas fir and the right para-rectal space. The patient´s post-operative course was marked by a good course with the completion of an obstetric control ultrasound showing an active intrauterine pregnancy with stable image of the trophoblastic detachment.
Formerly considered rare, heterotopic pregnancy is nowadays becoming more and more frequent with the advent of different assisted medical procreation techniques. Its overall incidence is estimated at 1/30000 in spontaneous pregnancies and varies between 1.5 per 1000 up to 1 per 100 in assisted pregnancies [2,3]. Beyond the factors linked to the various techniques of assisted medical procreation, other factors including tubal pathologies and a history of pelvic surgery or ectopic pregnancy are also incriminated in its occurrence [5]. The discovery may be sudden during the diagnosis of an apparently normal pregnancy or even in the context of the management of a first trimester bleeding. The existence of a heterotopic pregnancy with a progressive intrauterine pregnancy is associated with diagnostic difficulties. The clinical symptomatology dominated by the occurrence of abdominal pain and/or metrorrhagia as well as an increase in the serum concentration of chorionic gonadotropin (b-hCG) does not differ from the symptomatology in the event of threat of abortion and could lead to ignorance of heterotopic pregnancy [6]. Transvaginal ultrasound is essential for the diagnosis of heterotopic pregnancy, which presents as a coexisting intrauterine pregnancy with a separate adnexal mass or adnexal gestational sac [7]. However, this ultrasound has a low sensitivity, since the diagnosis of ectopic pregnancy may be missed or confused with a torsion of the appendix, a hemorrhagic cyst, a yellow body, a tubo-ovarian abscess or appendicitis [8,9]. The clinical picture of our patient was misleading with a diagnostic ambiguity on the etiology of the metrorrhagia for which she consulted. The ultrasound performed revealed the existence of a progressive intrauterine pregnancy with a trophoblastic detachment. In our present case, we carried out magnetic resonance imaging (MRI) given the difficulty we had in characterizing the lateral uterine image objectified by the initial ultrasound. MRI was not recommended in the diagnosis of a heterotopic pregnancy, but allowed us to know more about the adnexal image which was described on ultrasound. This image has been described by MRI as an ectopic pregnancy with a hematosalpinx. The Management is often difficult because the goal is to terminate the ectopic pregnancy by taking precautions to minimize the possible threat to intrauterine pregnancy [4]. Successful conservative therapy depends on rapid diagnosis, which can reduce the risk of life-threatening serious bleeding, hysterectomy, blood transfusion, and viable embryo death [10]. This management, which remains controversial, includes both surgical and medical management of the patient. Surgical treatment can confirm heterotopic pregnancy and evacuate ectopic pregnancy by laparoscopy or laparotomy [11]. The prognosis for intrauterine pregnancy is most often favorable.
Spontaneous heterotopic pregnancy remains rare and can occur apart from any other risk factor as it is the case in our observation. Transvaginal ultrasound, although useful for diagnosis, may not be specific. The use of pelvic MRI to diagnose our case was very helpful.
The authors declare no competing interests.
The authors participated in the care of the patient; writing and correcting the manuscript. All authors have read and approved the final version of the manuscript
Figure 1: lateral uterine image in favor of a hematosalpinx
Figure 2: trophoblastic detachment
- Talbot K, Simpson R, Price N, Jackson SR. Heterotopic pregnancy. J Obstet Gynaecol. 2011;31(1):7-12. PubMed | Google Scholar
- Govindarajan MJ, Rajan R. Heterotopic pregnancy in natural conception. J Hum Reprod Sci. 2008 Jan;1(1):37-8. PubMed | Google Scholar
- Barrenetxea G, Barinaga-Rementeria L, Lopez de Larruzea A, Agirregoikoa JA, Mandiola M, Carbonero K. Heterotopic pregnancy: two cases and a comparative review. Fertil Steril. 2007 Feb;87(2):417.e9-15. PubMed | Google Scholar
- Soriano D, Vicus D, Schonman R, Mashiach R, Shashar-Levkovitz D, Schiff E et al. Long-term outcome after laparoscopic treatment of heterotopic pregnancy: 19 cases. Journal of Minimally Invasive Gynecology. 2010;17(3):321-4. PubMed | Google Scholar
- Vargas RA, Leal R, Tijerina LO, Sepulveda DL. Heterotopic pregnancy: a case report. J Minim Invasive Gynecol. 2015;22(6S):S138. PubMed | Google Scholar
- Ertunc A, Beril Yuksel, Sermin Tok, Himmet Hatipoglu, Figen Aslan. Heterotopic pregnancy identified in the postpartum period. Int J Gynaecol Obstet. 2015 Sep;130(3):287-8. PubMed | Google Scholar
- Li XH, Ouyang Y, Lu GX. Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilization with embryo transfer. Ultrasound Obstet Gynecol. 2013;41(5):563e9. PubMed | Google Scholar
- Chen KH, Chen LR. Rupturing heterotopic pregnancy mimicking acute appendicitis. Taiwan J Obstet Gynecol. 2014;53(3):401e3. PubMed | Google Scholar
- Ezzati M, Shamshirsaz AA, Haeri S. Undiagnosed heterotopic pregnancy, maternal hemorrhagic shock, and ischemic stroke in the intrauterine fetus. Prenat Diagn. 2015;35(9):926e7. PubMed | Google Scholar
- Sepulveda González G, Villagómez Martínez GE, Basurto Diaz D, Guerra de la Garza Evia AR, Rosales de León JC, Arroyo Lemarroy T et al. Successful management of heterotopic cervical pregnancy with ultrasonographic-guided laser ablation. The Journal of Minimally Invasive Gynecology. May-Jun 2020;27(4):977-980. PubMed | Google Scholar
- Yiqi Guan, Caihong Ma. Clinical outcomes of patients with heterotopic pregnancy after surgical treatment. Journal of Minimally Invasive Gynecology. 2017;24(7):1111-5. PubMed | Google Scholar