Colonoscopy at a Tertiary Teaching Hospital in Ethiopia: a five-year retrospective review
Fikadu Girma Gudissa, Barecha Alemu, Samson Gebremedhin, Esayas Kebede Gudina, Hailemichael Desalegn
Corresponding author: Esayas Kebede Gudina, Department of Internal Medicine, Jimma University, Jimma, Ethiopia 
Received: 05 Oct 2020 - Accepted: 18 Jan 2021 - Published: 26 Jan 2021
Domain: Gastroenterology,Internal medicine
Keywords: Colonoscopy, colorectal cancer, diagnostic yield, Ethiopia, indication
©Fikadu Girma Gudissa et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Fikadu Girma Gudissa et al. Colonoscopy at a Tertiary Teaching Hospital in Ethiopia: a five-year retrospective review. PAMJ Clinical Medicine. 2021;5:37. [doi: 10.11604/pamj-cm.2021.5.37.26398]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/5/37/full
Colonoscopy at a Tertiary Teaching Hospital in Ethiopia: a five-year retrospective review
Fikadu Girma Gudissa1, Barecha Alemu1, Samson Gebremedhin2, Esayas Kebede Gudina3,&, Hailemichael Desalegn1
&Corresponding author
Introduction: colonoscopy is the gold standard procedure for diagnosing lower gastrointestinal disorders. However, it is relatively expensive and out of reach of many patients in resource limited settings. The objective of this study was to assess the common clinical indications, findings, and diagnostic yield of colonoscopy procedures performed at Saint Paul´s Hospital Millennium Medical College in Ethiopia.
Methods: medical records of randomly selected 309 participants were reviewed to collect background characteristics, indications and findings of colonoscopy procedures. Data were collected using structured and pretested case reporting format by trained clinicians.
Results: the mean age of the participants was 43.5 years (SD=15.67) with range of 15-84 years; 60.5% were male participants. The vast majority (95.1%) of colonoscopy indications were judged as appropriate. Evaluation for rectal bleeding (31.7%) and suspected colorectal cancer (15.2%) were the commonest indication for colonoscopy. However, screening colonoscopy for asymptomatic subjects was almost non-existent. The commonest colonoscopic findings were hemorroidal diseases (28.5%) and gross mass lesions (14.9%). The overall diagnostic yield was 74.1% being highest among patients presenting with lower gastrointestinal bleeding and bowel habit changes. About 58.3% of bowel preparations in this study were optimum but an excellent preparation was extremely low (13.3%).
Conclusion: our study revealed that colonoscopy procedures for symptomatic patients were performed for appropriate indications for most of the cases. However, screening colonoscopy was extremely low. The relatively high rate of abnormalities and malignant lesions in this finding calls for national strategy for early colonoscopy screening of high-risk population.
Colonoscopy is an extremely important and standard procedure in gastroenterology. It is an endoscopic examination of the large and the distal part of the small intestine with a fiber optic camera on a flexible tube passed through anal canal. Colonoscopy helps for visual diagnosis of ulcerations of intestinal mucosa, masses, and polyps. More importantly, it grants the opportunity for biopsy or removal of suspected colorectal cancer lesions [1,2]. Colon and rectum often host premalignant lesions and relatively easily accessible organs [3]. Endoscopic applications are the most efficient approaches used for executing mucosal pathologies in the gastrointestinal (GI) system including the colorectal diseases. In this regard, colonoscopy is an endoscopic procedure of choice for examination of the terminal ileal, colonic and rectal mucosa. It is considered the gold standard for diagnosing structural colonic diseases. Additionally, colonoscopy is the recommended follow-up procedure for positive Fecal Occult Blood Test (FOBT) and Flexible Sigmoidoscopy (FSIG). It is also used in the management and follow-up of patients with a range of clinical conditions including neoplastic, inflammatory and familial conditions [3-5].
Colonoscopy became increasingly popular from the 1970´s as useful diagnostic tool [6-8]. However, it was first recommended as a primary screening test for colorectal cancer (CRC) in 1997. This routine use of colonoscopy has reduced mortality and improved five-year cancer survival rate to 90% when the tumor is detected early by the help of colonoscopy [9,10]. Diseases like CRC are relatively common and easily detectable by colonoscopy. This makes CRC an important gastrointestinal cancer benefiting from screening colonoscopy [3,4]. Colonoscopy should be safe, complete, and comfortable and is effective both for diagnosis and therapeutic interventions. A principal benefit of colonoscopy is that it allows for a full structural examination of the bowel in a single session and for the removal or biopsy of lesions identified during the procedure. Other forms of colon investigation, if positive, usually require colonoscopy as a follow up procedure [3,4,11,12]. Colonoscopy is widely available throughout developed world in both public and private settings but there is scarcity of the procedure in many African countries including Ethiopia. As a result, publications on the use of colonoscopic studies as screening and diagnostic evaluation are almost non-existent. One study conducted over two decades ago revealed that rectal bleeding, bowel habit change and abdominal pain were major indications for colonoscopy in Ethiopia [13]. The aim of this study was to evaluate common clinical indications, findings, and diagnostic yield of colonoscopy at St. Paul´s Hospital, a tertiary teaching hospital in Addis Ababa, Ethiopia.
Study setting: this is a hospital based cross-sectional study conducted on medical records of patients who had colonoscopy examination during a period of 28th February 2014 to 1st March 2019 at St. Paul´s Hospital Millennium Medical College. St. Paul Hospital is one of the largest public tertiary teaching hospitals in Addis Ababa, Ethiopia. It is also one of the few public hospitals in the country that provide gastrointestinal endoscopy services. All the colonoscopy procedures at the hospital are performed either by a qualified gastroenterologist or a gastroenterology fellow supervised by a gastroenterologist. The endoscopy service was initially introduced at the hospital in 2008 and GI fellowship was started in 2015. The GI unit is now run by six gastroenterologists and one endoscopic surgeon. The endoscopy unit of St. Paul Hospital has recently been recognized by the World Endoscopy Organization (WEO) and European Society of Gastrointestinal Endoscopy (ESGE) as center for Endoscopy training. It is the first African center accredited by WEO as training center. The center plans to develop standard GI endoscopy services focusing on advanced interventional endoscopy and research.
Selection of study participants: during the period of 28th February 2014 to 1st March 2019, a total of 2,306 colonoscopies were performed. Out of these, 331 subjects were selected by using systematic random sampling technique. From the 331 cases selected for review, 22 were excluded based on exclusion criteria.
Data collection procedures: the medical records were reviewed to evaluate the indications, finding and diagnostic yield of colonoscopy. Individuals identified in the chart review to have undergone previous colonoscopy (having previous diagnosis); those with missing data, incomplete colonoscopy procedures, and unclear diagnosis/findings as well as those younger than < 15 years of age were excluded from the study. Appropriateness for colonoscopy was assessed by using American Society for Gastrointestinal Endoscopy (ASGE) criteria [14]. Indications for colonoscopy were considered as appropriate if the expected health benefits were judged to exceed the possible negative consequences by a sufficiently wide margin as assessed by appropriateness guideline. The diagnostic yield of the procedure was defined as detection of significant pathology in symptomatic subjects. Adequateness of bowel preparation was also assessed in accordance with the Boston Bowel Preparation Scale (BBPS) [15], a validated bowel preparation scale where scoring is performed for each segment of the colon: right colon (including cecum and ascending colon); transverse (includes hepatic and splenic flexures); and left colon (descending and sigmoid colon, and rectum).
The scale has a score of 0 to 9 points. Poor for score of 0, inadequate for score 1, good for score 2, and an excellent preparation for score of 3 were used. Based on BBPS, Score 0 - unprepared colon segment with mucosa not seen because of solid stool that cannot be cleared; score 1 - portion of mucosa of the colon segment seen, but other areas of segment not well seen because of staining, residual stool, and/or opaque liquid; score 2 - minor amount of residual staining, small fragments of stool, and/or opaque liquid, but mucosa of colon segment is well seen; and score 3- when the entire mucosa of colon segment is well seen, with no residual staining, small fragments of stool, or opaque liquid. Adequate (optimal) bowel preparation was defined as those reported as excellent, good or adequate (total score of ≥ 6 AND ≥ 2 per segment) and considered inadequate (sub optimal) for those reported as inadequate or poor. Reports of histopathological studies of specimens collected during colonoscopy were also reviewed. Data were collected using structured and pretested case reporting forms by trained clinicians. All available and complete records were included in the review.
Statistical analysis: the data were cleaned, edited, entered into and analyzed using the SPSS for windows version 20.0 statistical software (IBM SPSS®). Data was analyzed and presented using frequency distribution, graphs and charts.
Ethical considerations: relevant ethical clearance was obtained from St. Paul´s Hospital Millennium Medical College Institutional Review Board (IRB) and was delivered to the GI unit. To protect confidentiality of patient information, no identification was included in the data abstraction tool and access to the collected information was limited to the study team only.
Background characteristics of the study participants: of the 331 cases selected for review, 22 were excluded based on exclusion criteria. As a result, 309 subjects, 60.5% (187) male, were included in the study. The mean age was 43.3 years (SD =15.67) with range of 15 to 84 years; 37% were older than 50 years (Table 1).
Indications and appropriateness of colonoscopy examination: colonoscopy was complete in 289 (93.5%) of the patients and cecal intubation was not possible in 20 (6.5%) of cases due to obstructive mass (n=13), inadequate preparation (n=4), redundant colon (n=2) and fear of perforation (n=1). With regards to appropriateness of indications for colonoscopy, 294 (95.1%) were regarded as appropriate based on at least one ASGE criterion. The commonest indications for colonoscopy were bleeding per rectum 98 (31.7%) and evaluation for suspected colorectal cancer 47 (15.2%). In 82 (26.6%) of the cases, colonoscopy was indicated for change in bowel habits including unexplained chronic diarrhea 46 (14.9%) and recurrent constipation 36 (11.7%). Only 8.1% subjects underwent colonoscopy for screening of colorectal cancer and in fact, majority of these subjects had screening for pre-renal transplant work-up and searching for primary cancer after the diagnosis of cancer metastasis (Table 1).
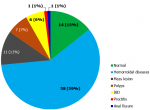
Colonoscopy findings and diagnostic yield: most of the examined subjects, 74.1% (229/309), had abnormal colonoscopic findings. Hemorroidal diseases 28.5% (88), gross mass lesions 14.9% (46), and inflammatory bowel diseases12.0% (37) were the most common abnormal findings. Moreover, 80 patients (25.9%) had normal colonoscopic studies (Table 2). The overall diagnostic yield of colonoscopy was 74.1% and with significant variability between different indications for it. The highest yields were observed in patients evaluated for rectal bleeding and chronic diarrhea with yields of 84.7% (83/98) and 73.9% (34/46) respectively. This indicates that lower GI bleeding and chronic diarrhea had highest diagnostic yield during the colonoscopy in this study. Among patients evaluated for lower GI bleeding, 59.2% (58/98) had hemorroidal diseases. Mass lesions (11.2%), polyps (7.2%) and inflammatory bowel disease (6.1%) were the other common findings in this group of patients (Figure 1).
Site of the lesions during colonoscopy examination: the distal colon was the commonest site involved with colonic pathologies. About 140(63.6%) pathologies were detected during the colonoscopy in this region of the colon. The anus and anal canal constituted for the majority in 89 (40.4%) of the cases and the recto-sigmoid region in 51 (23.2%) subjects. Findings of the other sites includes involvement of the whole colon in 9 (4.1%), terminal ilium in 8 (3.6%), the left colon including the recto-sigmoid and descending colon involved in 17 (7.7%), the right colon 15 (6.8%). More than one site was involved in some cases (Table 2).
Histopathology diagnosis: histopathology examination was performed for 114 patients. Analysis of the biopsy result showed that IBD 21.1% (24) and CRC 17.5% (20) were the commonest histopathology diagnosis followed by polyps 17.5% (20), and non-specific chronic inflammation 9.6% (11) (Table 2). About 27% (31) biopsy results were not accessible due to lost result or biopsy specimens were sent back to referring hospitals.
Site of colon involved in colorectal cancer: among the 20 subjects with colorectal cancer diagnosed on histopathology, 90% (18) were adenocarcinomas and the distal parts of the colon constituted for the majority 80% (15) -rectum 65% (13), anal canal 10%, and sigmoid colon 5%. About 70% of cases were diagnosed in male with mean age at diagnosis of 51.4 years (SD = 17.18) and age range of 16 to 82 years.
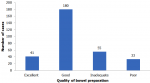
Quality of bowel preparation for colonoscopy examination: with regard to quality of bowel preparation, 180 (58.3%) subjects had good and 41 (13.3%) had excellent preparations. About one-fifth of the patients had sub-optimal bowel preparations. In About 17.8% (55) of the cases, their bowel preparation was inadequate and 33 (10.3%) had poor preparation (Figure 2).
Lower GI bleeding was found to be the commonest reason for colonoscopy examination at the hospital during the study period and hemorrhoidal diseases and mass lesions were the most common findings of the procedure. Generally, majority of the indications for colonoscopy were appropriate and vast majority of the procedures were complete. As colonoscopy is a relatively expensive and invasive procedure, its appropriateness should be judged based on its indication. Globally, 20-50% of colonoscopy procedures are done for inappropriate indications [16]. In this study, 95.1% of the colonoscopy procedures were performed for appropriate indications on at least one ASGE criterion. This figure is higher than many of the studies from both high-income settings [17-19] and low-income countries [20,21]. This difference could be attributed to the fact that majority of colonoscopy requests were screened for appropriateness by senior physicians working in the unit. Most of the patients were also symptomatic and were more likely to have clear indication for colonoscopy from the outset. The finding may also reflect that colonoscopy is not a common procedure in the country and only done for those with clear indications. Due to scarcity of the procedure in low income settings, colonoscopy is often limited to patients with overt GI symptoms. As a result, most patients who undergo this procedure have rectal bleeding, bowel habit change and abdominal pain as main indications [20-23]. Similarly, nearly one third of the indications for colonoscopy in this study were for rectal bleeding. Moreover, 58.3% of the reasons for colonoscopy were rectal bleeding and bowel habit changes (chronic diarrhea and constipation) a finding consistent with global data [19,21,23].
Conversely, there was very low rate of colonoscopy for routine screening in asymptomatic patients. Even in cases where colonoscopy was requested for screening purpose, it was not really for active screening but rather for searching for primary source of malignancy and for pre-renal transplant work up which was performed in 9.1% cases in our study. Along with lack of cancer control strategy, poor access to colonoscopy is one of the major barriers for colorectal cancer control in Africa [24,25]. The recent introduction of colonoscopy procedure in Ethiopia may have contributed to these findings in our study. This study showed that hemorrhoids were the commonest pathologies seen during colonoscopy accounting for 28.5%. Our finding is comparable with studies from Zambia, 26% [11], Pakistan, 36.2% [22] and Spain, 30.1% [19]. Hemorroidal diseases were also the commonest finding (59.2%) among patients presented with lower GI bleeding in this study. This finding is nearly comparable to study in Ghana where hemorrhoids accounts for 53% among patients presented with lower GI bleeding [26]. The diagnostic yield of 74.1% this study is almost identical with Zambian study that showed diagnostic yield of 74% [11]. In general, studies from Africa and other low- and middle-income countries [27-29] are known for higher yield as compared to those from high-income settings [18,30]. This difference could be explained partly by differences in indications, and by the fact that this study and other studies in low-income settings included symptomatic cases unlike studies from high-income settings where significant proportion had colonoscopy for CRC screening in asymptomatic cases. Diagnostic yield also varies based on appropriateness of the indications [30] and underlying symptoms being higher in those with bleeding and bowel habit change [31]. This study also revealed that diagnostic yield is highest in subjects who presented with bleeding per rectum (86.5% positive yield) and chronic unexplained diarrhea with 73.9% diagnostic yield (including non-bloody diarrhea). This finding is comparable with study from Sweden [31]. Nearly one-fourth (25.9%) of this study subjects had normal colonoscopic findings which is comparable with other studies [11,22].
With regard to site of lesions, most of the findings were in the distal colon-anal and recto-sigmoid region accounting for 63.6% of the pathologies. This observation of ano-rectal dominance was also reported from other African countries [32]. Similar to other sub-Saharan Africa [33], our study revealed that left-sided colon cancers were in the majority (80%) as opposed to the right shift in the Western countries [34]. Quality of bowel preparation plays an important role in improving diagnostic yield of colonoscopy. In our study, more than 70% of the patients had adequate bowel preparation (58.3% good and 13.3% excellent bowel preparation) which is lower than the high-income countries (79.2%) [35]. While many factors may contribute to this, the lack of standard bowel cleansing agent on local market is the most likely hindering factor. We believe that this study is one of the very few reports of its kind from Ethiopia and a reflection of clinical practice in the country especially in tertiary centers. All the procedures were performed by an experienced gastroenterologist and the findings can be used as baseline for further prospective investigations regarding indications, patterns of findings of colonoscopy, diagnostic yield, and correlation of the colonoscopy finding with histopathology diagnosis. However, our study is biased because of the fact that data was collected from only a single tertiary care center. As a result, inferences to the general population should be drawn cautiously given that these patients had clinical indications for colonoscopy in most instances. Moreover, the study was done based on retrospective collection of data from medical records. The loss of medical records might have hampered the quality of our data as a result.
Bleeding per rectum and bowel habit changes were the commonest indication for colonoscopy. Because the procedure was performed for symptomatic patients and those with clear indications, colonoscopy yield was found to be high. Though hemorriodal diseases were the commonest abnormalities detected, a significant proportion of those who underwent the procedure had serious underlying abnormalities including inflammatory bowel disease and colorectal cancer. Our finding also revealed that screening colonoscopy for asymptomatic patients was almost nonexistent. The findings also support the initial application of flexible sigmoidoscopy for investigating patients with suspected colorectal cancer and follow up colonoscopy for selected patients to exclude right sided pathology. The relatively high rate of abnormalities and malignant lesions in this finding calls for national strategy for early colonoscopic screening of high-risk population.
What is known about this topic
- Colonoscopy is an extremely important and standard procedure in gastroenterology; it is considered the gold standard for diagnosing structural colonic diseases;
- Routine screening for colorectal cancer using colonoscopy has dramatically reduced mortality and improved five-year cancer survival in high income countries;
- Colonoscopy remains highly inaccessible in most African countries.
What this study adds
- The yield of colonoscopy is high when it is used in patients with lower gastrointestinal symptoms;
- Colonoscopy is rarely used as pre-symptomatic screening for colorectal cancer in Africa despite increasing prevalence;
- Colonic lesions, particularly, colonic cancers are predominantly left sided as compared to predominantly right side in the developed world.
The authors declare no competing interests.
FGG designed the study, developed the instruments, supervised data collection, analyzed the data and wrote the manuscript. HD, BA, SG, and EKG participated in study design, instrument development, data analysis and writing of the manuscript. All authors have read and approved the manuscript in the current version.
We would like to express our heartily felt gratitude to the staffs of endoscopy units, pathology department and record officers for helping us during the data collection process and the St. Paul´s Hospital Millennium Medical College Administration and finance for funding the study.
Table 1: background characteristics and indications for colonoscopy in patients who underwent colonoscopy examination at St. Paul's Hospital Millennium Medical College (SPHMMC), Ethiopia (2014-2019)
Table 2: clonoscopic and histopathologic findings of patients who underwent colonoscopy at SPHMMC, Ethiopia (2014-2019)
Figure 1: colonoscopic findings among patients who underwent colonoscopy for indication of lower GI bleeding at SPHMMC, Ethiopia (2014-2019)
Figure 2: quality of bowel preparation among patients who underwent colonoscopic examinations at SPHMMC, Ethiopia (2014-2019)
- Waye JD. Colonoscopy. CA Cancer J Clin. 1992;42(6):350-65. PubMed | Google Scholar
- Lee SH, Park YK, Lee DJ, Kim KM. Colonoscopy procedural skills and training for new beginners. World J Gastroenterol. 2014;20(45):16984-95. PubMed
- Yanik S, Akkoca AN, Ozdemir ZT, Sozutek D, Yilmaz EE, Sayar S. Evaluation of results of lower gastrointestinal endoscopic biopsy. Int J Clin Exp Med. 2014;7(12):5820-5. PubMed | Google Scholar
- Akere A, Oke TO, Otegbayo JA. Colonoscopy at a tertiary healthcare facility in Southwest Nigeria: spectrum of indications and colonic abnormalities. Ann Afr Med. 2016;15(3):109-13. PubMed
- Wolff WI. Colonoscopy: history and development. Am J Gastroenterol. 1989;84(9):1017-25. PubMed | Google Scholar
- Wolff WI, Shinya H, Geffen A, Ozaktay SZ. Colonofiberoscopy: a new and valuable diagnostic modality. Am J Surg. 1972;123(2):180-4. PubMed | Google Scholar
- Waye JD. Colonoscopy. Surg Clin North Am. 1972;52(4):1013-24. PubMed | Google Scholar
- Shinya H, Wolff WI. Morphology, anatomic distribution and cancer potential of colonic polyps. Ann Surg. 1979;190(6):679-83. PubMed | Google Scholar
- Winawer SJ, Fletcher RH, Miller L, Godlee F, Stolar MH, Mulrow CD et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997;112(2):594-642. PubMed | Google Scholar
- Byers T, Levin B, Rothenberger D, Dodd GD, Smith RA. American cancer society guidelines for screening and surveillance for early detection of colorectal polyps and cancer: update 1997, American Cancer Society Detection and Treatment Advisory Group on Colorectal Cancer. CA Cancer J Clin. 1997;47(3):154-60. PubMed | Google Scholar
- Kayamba V, Nicholls K, Morgan C, Kelly P. A seven-year retrospective review of colonoscopy records from a single centre in Zambia. Malawi Med J. 2018;30(1):17-21. PubMed | Google Scholar
- Alatise OI, Arigbabu AO, Agbakwuru EA, Lawal OO, Ndububa DA, Ojo OS. Spectrum of colonoscopy findings in Ile-Ife Nigeria. Niger Postgrad Med J. 2012;19(4):219-24. PubMed | Google Scholar
- Kassa E. Colonoscopy in the investigation of colonic diseases. East Afr Med J. 1996;73(11):741-5. PubMed | Google Scholar
- American Society for Gastrointestinal Endoscopy. Appropriate use of gastrointestinal endoscopy, Gastrointest Endosc. 2000;52(6):831-7.
- Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69(3 Pt 2):620-5. PubMed | Google Scholar
- Telford JJ. Inappropriate uses of colonoscopy. Gastroenterol Hepatol (N Y). 2012;8(5):342-4. PubMed
- Harris JK, Froehlich F, Gonvers JJ, Wietlisbach V, Burnand B, Vader JP. The appropriateness of colonoscopy: a multi-center, international, observational study. Int J Qual Health Care. 2007;19(3):150-7. PubMed | Google Scholar
- Grassini M, Verna C, Niola P, Navino M, Battaglia E, Bassotti G. Appropriateness of colonoscopy: diagnostic yield and safety in guidelines. World J Gastroenterol. 2007;13(12):1816-9; discussion 9. PubMed | Google Scholar
- Marzo-Castillejo M, Almeda J, Mascort JJ, Cunillera O, Saladich R, Nieto R et al. Appropriateness of colonoscopy requests according to EPAGE-II in the Spanish region of Catalonia. BMC Fam Pract. 2015;16:154. PubMed | Google Scholar
- Ugiagbe R, Omuemu C, Imarhiagbe FA. Appropriateness of indication and diagnostic yield of colonoscopy in a southern Nigerian tertiary hospital. BJMMR. 2016;14(8):8. PubMed | Google Scholar
- Samarakoon Y, Gunawardena N, Pathirana A, Hewage S. "Appropriateness of colonoscopy according to EPAGE II in a low resource setting: a cross sectional study from Sri Lanka". BMC Gastroenterol. 2018;18(1):72. PubMed | Google Scholar
- Rehman KU, Qureshi MO, Khokhar N, Shafqat F, Salih M. Quality of colonoscopy and spectrum of lower gastrointestinal disease as determined by colonoscopy. J Coll Physicians Surg Pak. 2015;25(7):478-81. PubMed | Google Scholar
- Olokoba AB, Obateru OA, Bojuwoye MO, Olatoke SA, Bolarinwa OA, Olokoba LB. Indications and findings at colonoscopy in Ilorin, Nigeria. Niger Med J. 2013;54(2):111-4. PubMed | Google Scholar
- Laiyemo AO, Brawley O, Irabor D, Boutall A, Ramesar RS, Madiba TE. Toward colorectal cancer control in Africa. Int J Cancer. 2016;138(4):1033-4. PubMed
- May FP, Anandasabapathy S. Colon cancer in Africa: primetime for screening. Gastrointest Endosc. 2019;89(6):1238-40. PubMed | Google Scholar
- Dakubo J, Kumoji R, Naaeder S, Clegg-Lamptey J. Endoscopic evaluation of the colorectum in patients presenting with haematochezia at korle-bu teaching hospital Accra. Ghana Med J. 2008;42(1):33-7. PubMed | Google Scholar
- Dinesh HN, Shashidhar HB, Prasad V. An analysis of colonoscopy findings in a tertiary care hospital. Int J Sci Stud. 2015;3(7):5.
- Ray-Offorf E, SEB I. Diagnostic yield of colonoscopy. J Clin Gastroenterol Hepatol. 2018;2(2):4.
- Parekh D, Malpathak V. Role of colonoscopy in diagnosis of lower gastro-intestinal diseases. MVP Journal of Medical Sciences. 2017;4(2):6. Google Scholar
- Morini S, Hassan C, Meucci G, Toldi A, Zullo A, Minoli G. Diagnostic yield of open access colonoscopy according to appropriateness. Gastrointest Endosc. 2001;54(2):175-9. PubMed | Google Scholar
- Lasson A, Kilander A, Stotzer PO. Diagnostic yield of colonoscopy based on symptoms. Scand J Gastroenterol. 2008;43(3):356-62. PubMed | Google Scholar
- Ajayi A, Ajayi EA, Solomon OA and Udo E. Lower gastrointestinal bleeding: spectrum of colonoscopy findings in Ado-Ekiti, Nigeria. Int J Med Sci. 2014;6(5):128-33. Google Scholar
- Graham A, Adeloye D, Grant L, Theodoratou E, Campbell H. Estimating the incidence of colorectal cancer in sub-Saharan Africa: a systematic analysis. J Glob Health. 2012;2(2):020404. PubMed | Google Scholar
- Saltzstein SL, Behling CA. Age and time as factors in the left-to-right shift of subsite of colorectal adenocarcinoma: a study of 213,383 cases from the California cancer registry. J Clin Gastroenterol. 2007;41(2):173-7. PubMed | Google Scholar
- Clark B, Protiva P, Nagar A, Imaeda A, Ciarleglio MM, Deng Y et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405. PubMed | Google Scholar