Trachoma in a one-eyed patient: case report
Rida El Hadiri, Rim El Hachimi, Amine Ennejjar, Nourdine Boutimzine, Abdellah Amazouzi, Lalla Ouafa Cherkaoui
Corresponding author: Rida El Hadiri, Université Mohammed V de Rabat, Centre Hospitalier Universitaire Ibn Sina, Hôpital des Spécialités, Ophtalmologie A, Rabat, Morocco 
Received: 23 Oct 2021 - Accepted: 21 Nov 2021 - Published: 06 Dec 2021
Domain: Ophthalmology
Keywords: Trachoma, infection, corneal ulcer, dry eye disease, case report
©Rida El Hadiri et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Rida El Hadiri et al. Trachoma in a one-eyed patient: case report. PAMJ Clinical Medicine. 2021;7:20. [doi: 10.11604/pamj-cm.2021.7.20.32150]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/7/20/full
Trachoma in a one-eyed patient: case report
![]() Rida El Hadiri1,&,
Rida El Hadiri1,&, ![]() Rim El Hachimi1, Amine Ennejjar,1, Nourdine Boutimzine1, Abdellah Amazouzi1,
Rim El Hachimi1, Amine Ennejjar,1, Nourdine Boutimzine1, Abdellah Amazouzi1, ![]() Lalla Ouafa Cherkaoui1
Lalla Ouafa Cherkaoui1
&Corresponding author
Trachoma is a bacterial infectious disease that may cause blindness. We report a case of chronic stage of trachoma complicated by a corneal ulcer. Epidemiological and clinical clues lead to the diagnosis in a patient complaining of a chronic foreign body sensation, blurred vision and tearing OS. His medical history was positive for recurrent episodes of red eye and purulent discharges self-managed by Aureomycin ointment with a past palpebral surgery orbital septum (OS) and severe ocular trauma OD. This case was managed medically with fair outcome. We will highlight interesting clinical, therapeutical and socio-economic challenges that may present this old but severe disease.
Trachoma is a disease characterized by recurrent ocular infections with obligate intracellular bacteria called Chlamydia trachomatis [1]. This old disease is still the leading infectious cause of blindness worldwide and is foremost a disease of poverty with deprivation of proper sanitation and clean water [2-3]. Repeated episodes of active disease occur particularly during childhood leading to various degrees of distress. Diagnosis could be made on the basis of clinical signs in endemic areas [4-5]. Morocco had been successful in achieving elimination goals and had moved to the surveillance phase but practitioners still face different aspects of this infectious disease [6]. Herein, we report the case of a cicatricial trachoma with a multi-etiological dry eye and aseptic corneal ulcer illustrating the severity of this condition that still a sight-threatening disease.
Patient Information: it was a 72-year-man who consulted for foreign body sensation, blurred vision and tearing for two years. The patient originated from a province in south-western Morocco. He was illiterate and of low socioeconomic status. His medical history was positive for recurrent episodes of red eye and purulent discharges self-managed by Aureomycin ointment. He also reported a severe contusive traumatism to her right eye leading to phthisis bulbi and eyelid surgery of the left eye.
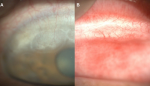
Clinical Findings: on examination, visual acuity was no light perception OD and 1m counting fingers OS, pupils were reactive, IOP was 15mmHg and ocular motility was full. We noted horizontal eyelid laxity without eyelid or eyelash malposition. Slit lamp evaluation showed the presence of posterior blepharitis, white sheets of fibrosis in the superior tarsal conjunctiva, superior vascular corneal pannus and limbal depressions corresponding to Herbert pits (Figure 1 A,B). On the inferonasal area, we found a pentagon shaped ulcer with a central pit highlighted by pooling of fluorescein (Figure 2 A,B). Besides, we noted an inferior punctuate keratitis, decreased Tear break-up time, a dense subcapsular cataract and inaccessible fundus examination. Axial length was 29.34mm.
Diagnosis: we conclude to a case of cicatricial trachoma in presence of typical clinical findings with a dry eye disease mainly due to trachoma and meibomian gland dysfunction complicated by a corneal ulcer.
Therapeutic interventions: the patient was managed by warm compresses, eyelid hygiene and massage with application of topical preservative free lacrymal substitutes. We also insisted on facial cleanliness and environmental control to avoid reinfections. After four months, the patient was scheduled for a keratoplasty combined with cataract surgery but he refused to undergo any surgical procedure.
Follow-up and outcome of interventions: after four months, we noted a significant relief of symptoms with amelioration of the tear breakup time (TBUT) and disparition of corneal staining with persistent corneal ulcer. Herein, the patient was scheduled for a keratoplasty combined with cataract surgery but he refused to undergo any surgical procedure.
Trachoma is a preventable affection recognized for millennia but yet, many aspects still incompletely elucidated regarding its pathogenesis, diagnosis and management. Morocco had been successful in achieving elimination goals and had moved to the surveillance phase but practitioners still face different aspects of this infectious disease [6]. Acute and chronic manifestations could coexist in the same individual because of recurrent infections. Our patient had chronic stage of trachoma secondary to recurrent episodes of active infection. We found that eyelid surgery was of paramount importance to prevent potentially blinding complications especially in a one-eyed cataract patient with low socioeconomic status. This case illustrates classical signs found in late-stage trachoma with conjunctival scarring, corneal pannus, Herbert pits and a pentagon shaped ulcer probably related to a previous eyelid malposition. Dry eye had multiple risk factors including Meibomian gland dysfunction, conjunctival scaring and previous eyelash malposition. Every ophthalmologist should be able to recognize and manage patient suffering from this disease. Personal and collective efforts should be intensified and maintained to prevent and face this complex pathology.
Trachoma is still present in our daily practice and should be properly recognized and managed by young ophthalmologists. In chronic stages, it may severely compromise the anatomical and functional prognosis of the affected patients as illustrated by our case. Thus, we insist on the importance of emphasizing prevention and maintaining global awareness regarding this face with multiple masks.
The authors declare no competing interest.
Rida El Hadiri; did the final draft, Rim El Hachimi, Amine Ennejjar; did the bibliographic search, Nourdine Boutimzine, Abdellah Amazouzi, Lalla Ouafa Cherkaoui; did the corrections and contributions. All the authors read and agreed to the final manuscript.
Figure 1: (A) slit lamp pictures of the the left eye showing superior vascular corneal pannus and Herbert pits; (B) with white sheets of fibrosis in the tarsal conjunctiva
Figure 2: (A) slit lamp pictures of the the left eye showing pentagon shaped ulcer with a central pit; (B) highlighted by pooling of fluorescein
- Mohammadpour M, Abrishami M, Masoumi A, Hashemi H. Trachoma: past, present and future. J Curr Ophthalmol . 2016 Sep 19;28(4):165-169. PubMed | Google Scholar
- Mufioz B, West S. Trachoma: the forgotten cause of blindness. Epidemiol Rev. 1997;19(2):205e217. PubMed | Google Scholar
- Stocks ME, Ogden S, Haddad D, Addiss DG, McGuire C, Freeman MC. Effect of water, sanitation, and hygiene on the prevention of trachoma: a systematic review and meta-analysis. PLoS Med. 2014 Feb 25;11(2):e1001605. PubMed | Google Scholar
- Solomon AW, Peeling RW, Foster A, Mabey DC. Diagnosis and assessment of trachoma. Clin Microbiol Rev . 2004 Oct;17(4):982-1011. PubMed | Google Scholar
- Mathew AA, Turner A, Taylor HR. Strategies to control trachoma. Drugs . 2009 May 29;69(8):953-70. PubMed | Google Scholar
- Hammou J, Obtel M, Razine R, Berraho A, Belmekki M. Elimination of trachoma from Morocco: a historical review. East Mediterr Health J . 2020 Jun 24;26(6):713-719. PubMed | Google Scholar