Management of delayed post-traumatic tension pneumoventricle in a resource-limited setting: a report of two cases
Ousmane Issoufou Hamma, Ousmane Aboubacar Idrissa, Mahamane Mobarak Salifou Abdou, Avocefohoun Chanel Angelo, Sahidou Sani Mato, Souleymane Mahamadou Ango
Corresponding author: Ousmane Issoufou Hamma, Department of Neurosurgery, National Hospital of Niamey, Niamey, Niger 
Received: 19 Mar 2024 - Accepted: 02 Apr 2024 - Published: 04 Apr 2024
Domain: Neurosurgery
Keywords: Pneumocephalus, craniocerebral trauma, cerebrospinal fluid rhinorrhea, developing countries, case report
©Ousmane Issoufou Hamma et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Ousmane Issoufou Hamma et al. Management of delayed post-traumatic tension pneumoventricle in a resource-limited setting: a report of two cases. PAMJ Clinical Medicine. 2024;14:37. [doi: 10.11604/pamj-cm.2024.14.37.43330]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/14/37/full
Case report 
Management of delayed post-traumatic tension pneumoventricle in a resource-limited setting: a report of two cases
Management of delayed post-traumatic tension pneumoventricle in a resource-limited setting: a report of two cases
![]() Ousmane Issoufou Hamma1,&, Ousmane Aboubacar Idrissa1, Mahamane Mobarak Salifou Abdou2, Avocefohoun Chanel Angelo1, Sahidou Sani Mato1,
Ousmane Issoufou Hamma1,&, Ousmane Aboubacar Idrissa1, Mahamane Mobarak Salifou Abdou2, Avocefohoun Chanel Angelo1, Sahidou Sani Mato1, ![]() Souleymane Mahamadou Ango1
Souleymane Mahamadou Ango1
&Corresponding author
Delayed post-traumatic pneumoventricle tension is characterized by a pathological accumulation of air in the cerebral ventricles after 72 hours of head trauma. This is a rare neurosurgical emergency that occurs following a skull base fracture complicated by an osteodural defect without pneumocephalus or, more rarely, as a complication of simple acute post-traumatic pneumoventricle. This is a challenge in low-income countries due to limited access to brain imaging and neurosurgical technical platforms. Its management requires serial brain imaging from the acute phase of trauma. We report two patients with head trauma whose state of consciousness deteriorated after they returned home following rhinorrhea recurrence. Emergency computed tomography revealed a delayed post-traumatic tension pneumoventricle. Despite our limited resources, rapid intervention has led to favorable outcomes. Our aim was to show that recurrent rhinorrhea is an important sign to consider in patients with skull base trauma in the context of limited resources.
Pneumocephalus is defined as the presence of air in the epidural, subarachnoid, intraparenchymal, or intraventricular space (pneumoventricle) [1-3]. The pneumoventricle is mainly observed after intracranial surgery, and skull base pathology complicated by an osteodural defect, which is particularly traumatic or sometimes spontaneous [4,5]. Posttraumatic tension pneumoventricle is an extremely rare neurosurgical emergency that occurs 72 hours after head trauma. It occurs after a skull base fracture complicated by an osteodural defect without pneumocephalus or, more rarely, as a complication of a simple post-traumatic pneumoventricle [1,3,6,7]. This is a challenge in low-income countries due to limited access to brain imaging and neurosurgical technical platforms. Its management requires serial brain imaging from the acute phase of trauma. We report two patients with head trauma whose state of consciousness deteriorated after they returned home following rhinorrhea recurrence. Emergency Computed tomography (CT) revealed a delayed post-traumatic tension pneumoventricle. Despite our limited resources, rapid intervention has led to favorable outcomes. Rhinorrhea recurrence is therefore an important sign to consider in the event of skull base fracture in the context of limited resources.
Patient 1
Patient information: a 36-year-old farmer was referred to us in an emergency for secondary deterioration in his state of consciousness associated with rhinorrhea and fever. He had suffered severe head trauma with immediate coma and rhinorrhea a fortnight earlier, following a head-on collision with another motorcyclist. He was then transported to a peripheral health center where he received medical treatment involving nasal tamponade, which improved his clinical condition, after which he returned to consciousness 12 hours later. After five days, the patient had left the hospital in good general condition, but minimal headache persisted. He had not undergone a brain computed tomography (CT) scan because of financial constraints. Twelve days later, he was readmitted to this center because of progressive deterioration in his state of consciousness, the reappearance of rhinorrhea, and fever. He was quickly transferred to our hospital, which is approximately 200 km away, for further treatment.
Clinical findings: on admission, the patient was obnubilate with a Glasgow Coma Scale (GCS) score of 12/15 (Y3 V4 M5). His pupils were symmetrical and reactive to light. He was hemodynamically and ventilatorically stable, with a pulse rate of 96 beats/min, respiratory rate of 20 beats/min, and blood pressure of 105/75 mmHg; however, he had a fever of 39°C. The patient had intracranial hypertension syndrome with headache, vomiting, and meningeal stiffness but no neurological deficits. He also presented with clear cerebrospinal rhinorrhea and palpebral ecchymosis.
Diagnostic assessment: cerebral computed tomography (CT) revealed an extensive tension pneumoventricle with a mass effect associated with a diffuse pneumocephalus subarachnoid with an “air bubble sign” and a fracture of the right orbit roof (Figure 1). Cerebrospinal fluid (CSF) examination revealed signs of meningitis, with hypercellularity of 200 leukocytes/mm3 predominantly neutrophilic, hyperproteinorachia greater than 1 g/L, and normal glycorrhachia. Blood work revealed signs of infection, with an accelerated erythrocyte sedimentation rate (ESR) of 60 mm/h, C-reactive protein (CRP) levels greater than 6 mg/L, and hyponatremia of 118 mmol/L.
Diagnosis: the results were consistent with a pneumoventricle complicated with meningitis.
Therapeutic interventions: the patient received preoperative treatment for meningitis, including fluid and electrolyte rehydration and empirical antibiotic therapy (ceftriaxone 4 g/24 h, metronidazole 500 mg/8 h, and gentamicin 160 mg/24 h). The patient was rapidly taken to the operating room for surgical decompression via aspiration of the pneumoventricle and repair of the osteodural defect via a pterional approach (Figure 2). A right frontobasal dural defect was observed intraoperatively. An external ventricular drain was placed in the anterior horn of the right lateral ventricle to evacuate air, and the frontobasal dural defect was repaired (Figure 3). The mucosa of the right frontal sinus was cauterized and then filled with bone wax soaked in 10% dermal betadine.
Follow-up and outcome of interventions: the postoperative course was straightforward, and the patient gradually regained consciousness. He no longer had headaches or cerebrospinal rhinorrhea but developed bilateral hyposmia, which was treated with a short course of corticosteroids (prednisolone 1 mg/kg) for one week. Parenteral antibiotic therapy was maintained until ESR and CRP levels normalized (for 21 days). He was discharged on day 22 and was followed up as an outpatient for three months. At his last visit, he reported no rhinorrhea recurrence and only mild hyposmia.
Patient perspective: “I feel good”
Informed consent: the patient provided informed consent.
Patient 2
Patient information: a 40-year-old illegal gold digger presented with worsening consciousness and intense frontal headache. He had suffered a head injury with an initial loss of consciousness five days earlier following the collapse of his gold mining shaft. After being extricated from the shaft, the patient presented with multiple skin abrasions all over his body, headache, and rhinorrhagia, but no obvious serious injuries. However, he returned home without consulting a health center and treated his pain by self-medication. Four days later, he experienced intracranial hydroaeric noises when he blew his nose forcefully, followed by an intensification of his headache and rhinorrhagia. On the same day, his consciousness progressively deteriorated, prompting his consultation at our center, which is located approximately 300 km from his home.
Clinical findings: at admission, he was drowsy with a GCS score of 13/15 (Y3 V4 M6) and was hemodynamically and ventilatorically stable, with a pulse rate of 86 beats/min, respiratory rate of 14 beats/min, and blood pressure of 125/80 mmHg. He had no fever. The patient presented with intracranial hypertension syndrome consisting of intense headaches and visual disturbances. He also had abundant clear cerebrospinal rhinorrhea.
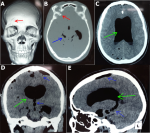
Diagnostic assessment: cerebral CT revealed an extensive tension pneumoventricle with a mass effect associated with diffuse subarachnoid pneumocephalus with an “air bubble sign” and ethmoid fracture (Figure 4). There was also excessive pneumatization of the ethmoid cells. The biological examination was unremarkable, and the CSF examination was normal.
Diagnosis: the results were consistent with a pneumoventricle.
Therapeutic interventions: conservative treatment was indicated, and the patient was placed on strict bed rest in the 30° Fowler position, with avoidance of any Valsalva maneuvers (coughing and sneezing) and 100% high-flow oxygen therapy (5 liters/min) for 72 h. He received hydroelectrolytic rehydration (2 liters/24 h) with progressive correction of natremia, analgesics (paracetamol 500 mg/8 h and acupan 20 mg/8 h), osmotherapy (mannitol 0, 5 mg/kg/8 h) for 48 h, antibiotic prophylaxis (ceftriaxone 4 g/24 h) for 72 hours, pneumococcal vaccination (pentavalent), and repeated lumbar puncture 50 cc/12 h until rhinorrhea stopped.
Follow-up and outcome of intervention: patient pain improved within the first few days. Her cerebrospinal rhinorrhea stopped after 96 hours. No complications were reported during hospitalization, and the patient was discharged on day 14 with instructions to avoid any Valsalva maneuvers. He was followed up as an outpatient for six months, with no clinical signs of recurrence.
Patient perspective: “I feel well”
Informed consent: the patient provided informed consent.
Posttraumatic tension pneumoventricles have rarely been reported in the scientific literature [1,7-9]. We were unable to determine exactly how this pathology developed in our patients because none of them underwent successive brain imaging from the acute phase of the trauma (> 72 hours). However, we assume that our second patient (patient 2) developed a simple acute post-traumatic pneumoventricle, which subsequently worsened, given the evolution of his clinical picture. Moreover, cases of secondary worsening of the pneumoventricle are the most frequently reported [1,2,6,8]. Monitoring the persistence or reappearance of post-traumatic cerebrospinal rhinorrhea is essential because it is one of the first signs of worsening clinical conditions, as we observed in our patients. In addition, certain skull base abnormalities, such as congenital bony malformations (paranasal sinus pneumoceles, pneumosinus, ethmoidal meningocele), previous skull base surgery, ventricular approaches, and tumors, may increase the risk of post-traumatic tension pneumoventricle [1,2,4,5,8].
On the pathophysiological level, the tension pneumoventricles are similar to other types of tension pneumocephalus and can be explained by two mechanisms. The first is the inverted soda bottle mechanism, where air is drawn into the cranial compartment by the negative pressure created by the flow of CSF through an osteodural defect (cerebrospinal rhinorrhea or cerebrospinal otorrhea). The second mechanism is the ball valve mechanism, in which air enters the skull unilaterally through an osteodural defect with high pressure created by the Valsalva maneuver (coughing, sneezing, blowing the nose). The air is then trapped intracranially, increasing the intracranial pressure [1,3-6]. The accumulation of this air is at the root of the clinical manifestations presented by patients, including persistent headache, vomiting, intracranial hydroareic noises perceived by patients, seizures, frontal syndrome, deterioration of consciousness, and even a state of coma (requiring emergency surgical decompression) [1,4,7]. The presence of air in the posterior cerebral fossa can lead to signs of brainstem damage and neurovegetative disorders; however, none of our patients showed these signs [3].
Cerebral computed tomography (CT) is the gold standard for diagnosing tension pneumocephalus [3,5,6]. However, post-traumatic tension pneumoventricle may require precise preoperative localization of the osteodural defect. The latter is generally located at the base of the skull and is revealed by high-resolution CT or T2 cisternography magnetic resonance imaging (MRI) alone or coupled with high-resolution CT [5,6]. Unfortunately, in low-income countries, access to these brain imaging methods remains difficult because of the insufficient number or absence of high-field MRI machines and the absence of social security to cover the high cost of these examinations, which cost several times the minimum wage, making management difficult.
As in the case of our second patient (patient 2), conservative treatment can be considered a first-line treatment for seven days, with close monitoring when neurological status permits. However, surgery is necessary in the event of signs of encephalic involvement or persistent minimal post-traumatic cerebrospinal rhinorrhea lasting more than ten days or if rhinorrhea recurrence. Surgical repair of the osteodural defect is required to avoid recurrence after conservative treatment or encephalic infection [8,10]. In our department, we routinely include osmotherapy and repeated lumbar puncture (100 to 200 cc/d) as conservative treatments, particularly when cerebrospinal rhinorrhea is not negligible. However, cases of pneumocephalus aggravated by lumbar subtraction of the CSF have been reported [4]. External ventricular drainage with external air aspiration is a simple, less invasive technique for the emergency management of a tension pneumoventricle that is not associated with rhinorrhea [4,6]. Endoscopic osteodural repair involves less morbidity than open surgery; however, few neurosurgical departments in our region have such technical equipment [5]. Notably, regardless of the surgical technique used, pneumocephalus generally progresses well when the diagnosis and management are early and high-quality.
Delayed post-traumatic tension pneumoventricle is a major and potentially fatal complication following skull base fracture. It can occur after hospital discharge, especially if rhinorrhea recurrence. Despite our limited resources, our patients have progressed well thanks to prompt management. Rhinorrhea recurrence is therefore a major sign to watch out for in patients followed up for skull base trauma in the context of limited resources.
The authors declare no competing interests.
Patient management: Ousmane Issoufou Hamma, Ousmane Aboubacar Idrissa, Avocefohoun Chanel Angelo, Sahidou Sani Mato and Souleymane Mahamadou Ango. Data collection: Ousmane Issoufou Hamma, Avocefohoun Chanel Angelo, and Ousmane Aboubacar Idrissa. Manuscript drafting: Ousmane Issoufou Hamma, Avocefohoun Chanel Angelo, and Mahamane Mobarak Salifou Abdou. Manuscript revision: Ousmane Issoufou Hamma and Mahamane Mobarak Salifou Abdou. All authors have approved the final version of the manuscript.
Figure 1: computed tomography images showing: (A,B) the left frontal fracture taking the anterior stage of the skull base (red arrow); (C,D,E) the pneumoventricle (green arrow); and the diffuse subarachnoid pneumocephalus (blue arrow)
Figure 2: image after installation in the operating theater showing the incision line (white arrow)
Figure 3: intraoperative images showing: (A) the creation of the bone flap; (B) the dural defect and opening of the left frontal sinus
Figure 4: competed tomography images showing: (A,B,C,D,E) the pneumoventricle (green arrow); the subarachnoid diffuse pneumoventricle (blue arrow); (B,F) and the skull base fracture (red arrow)
- Dabdoub C, Salas G, Silveira E doN, Dabdoub C. Review of the management of pneumocephalus. Surg Neurol Int. 2015 Sep 29:6:155. PubMed | Google Scholar
- De Jesus O, Thomas RJF de, Feliciano C. Tension pneumoventricle in a patient with a ventriculoperitoneal shunt and an ethmoidal meningoencephalocele. Surg Neurol Int. 2022 May 13;13:202. PubMed | Google Scholar
- Mirkarimi T, Salek M, Modirian E, Namdar P. Delayed post-traumatic Tension Hydropneumocephalus; a Case Report of Conservative Treatment. Arch Acad Emerg Med [Internet]. 2021 Feb 27;9(1):e22. PubMed | Google Scholar
- Almubarak AO, Fakhroo F, Alhuthayl MR, Kanaan I, Aldahash H. Tension Pneumoventricle Secondary to Cutaneous-Ventricular Fistula: Case Report and Literature Review. World Neurosurg. 2020 Oct;142:155-8. PubMed | Google Scholar
- Lefranc M, Peltier J, Demuynkc F, Bugnicourt JM, Desenclos C, Fichten A et al. Tension pneumocephalus and rhinorrhea revealing spontaneous cerebrospinal fluid fistula of the anterior cranial base. Neurochirurgie. 2009 Jun;55(3):340-4. PubMed | Google Scholar
- Shaikh N, Chanda A, Hassan J, Al-Kubaisi A, Momin U, Alyafai A. Tension pneumoventricle: Reversible cause for aphasia. Qatar Med J. 2021 Apr 23;2021(1):15. PubMed | Google Scholar
- Kankane V, Jaiswal G, Gupta T. Posttraumatic delayed tension pneumocephalus: Rare case with review of literature. Asian J Neurosurg. 2016 Dec;11(04):343-7. PubMed | Google Scholar
- Rajan VTT, Dharini GK, Anand VSS, Nandish HS. When Mount Fuji Can Erupt after Seven Days: A Case Report of Delayed Posttraumatic Tension Pneumocephalus with Literature Review. J Neurosci Rural Pract . 2020 Mar 3;11(1):187-90. PubMed | Google Scholar
- Ani CC, Ismaila BO. Tension pneumoventricle: A report of two cases. Niger J Clin Pract. 2016 Aug;19(4):559. PubMed | Google Scholar
- Kwon J, Rha HK, Park HK, Chough CK, Joo WI, Cho SH et al. Proper Management of Posttraumatic Tension Pneumocephalus. Korean J Neurotrauma. 2017;13(2):158. PubMed | Google Scholar