Nasopharyngeal tuberculosis: report of two cases
Anouar Ben Ameur El Youbi, Mariam Ameziane Hassani, Abdellatif Oudidi, Nawal Hammas, Mohamed Noureddine EL Alami El Amine
Corresponding author: Department of Otolaryngology and Cervicofacial Surgery, Hassan II University Hospital, Fes, Morocco 
Received: 02 Apr 2024 - Accepted: 05 Apr 2024 - Published: 16 Apr 2024
Domain: Head, Neck and Reconstructive Surgery,Otolaryngology (ENT)
Keywords: Tuberculosis, nasopharyngeal, lymphadenopathy
©Anouar Ben Ameur El Youbi et al. PAMJ Clinical Medicine (ISSN: 2707-2797). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Anouar Ben Ameur El Youbi et al. Nasopharyngeal tuberculosis: report of two cases. PAMJ Clinical Medicine. 2024;14:40. [doi: 10.11604/pamj-cm.2024.14.40.43489]
Available online at: https://www.clinical-medicine.panafrican-med-journal.com//content/article/14/40/full
Nasopharyngeal tuberculosis: report of two cases
![]() Anouar Ben Ameur El Youbi1&,
Anouar Ben Ameur El Youbi1&, ![]() Mariam Ameziane Hassani1, Abdellatif Oudidi1, Nawal Hammas2, Mohamed Noureddine EL Alami El Amine1
Mariam Ameziane Hassani1, Abdellatif Oudidi1, Nawal Hammas2, Mohamed Noureddine EL Alami El Amine1
&Corresponding author
In Morocco, tuberculosis poses a significant public health problem. Nasopharyngeal tuberculosis is a rare condition that presents diagnostic and therapeutic challenges. In this study, we focus on this condition by describing the clinical observations of two patients diagnosed with nasopharyngeal tuberculosis. One aged 28-year-old and the other 51-year-old. The first presented with lymphadenopathy, while both patients presented with rhinological symptoms. Histopathological examination of biopsies confirmed the diagnosis of nasopharyngeal tuberculosis. Both patients were referred to the pneumo-phtisiology department to initiate anti-tubercular antibiotic treatment. They both showed good clinical improvement. Nasopharyngeal tuberculosis is a rare but important condition to recognize. It presents diagnostic challenges due to its similarity to neoplastic pathologies. The prognosis with anti-tubercular treatment is generally good, with treatment failure mainly attributed to the emergence of multi-drug resistant strains.
Tuberculosis is a specific infectious disease caused by the Koch bacillus. It can manifest as primary infection through inhalation or secondary to hematogenous dissemination from another site [1]. Although tuberculosis can affect various organs, otorhinolaryngology localizations are relatively rare, and localization in the nasopharynx is even rarer [2]. Symptoms often mimic those of a malignant tumor [3], and the definitive diagnosis is established through histology [4,5]. We report two cases of nasopharyngeal tuberculosis, confirmed by histopathological study after nasopharyngeal biopsies. Both patients were placed on anti-tubercular treatment.
Observation 1
Patient information: a 28-year-old female with no significant medical history, presenting with chronic lateral cervical lymphadenopathy over 6 months associated with bilateral nasal obstruction.
Clinical findings: on general examination, the patient is in good general condition. Cervical examination revealed the presence of hard, mobile, painless lateral cervical lymphadenopathy, measuring up to two cm in the greatest diameter at the middle jugular-carotid level on the left side, without signs of inflammation. Rhinological examination revealed an inflamed mucosa, with nasal obstruction more pronounced on the right side. Nasofibroscopy was performed, revealing a budding process filling the fossa of Rosenmüller.
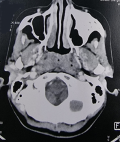
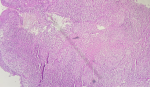
Diagnostic and assessment: due to suspicion of malignancy, a computed tomography (CT) scan was requested, revealing irregular and extensive tissue thickening of the postero-lateral walls of the nasopharynx, largely obstructing the rhino pharyngeal lumen, measuring 30mm in the greatest axis (Figure 1). This was associated with necrotic rhino pharyngeal and later cervical lymphadenopathies. The patient first underwent multiple biopsies of the nasopharynx. Subsequently, she underwent an exploratory cervicotomy with excision of the left middle jugulo-carotid lymph node. Histopathological examination of the nasopharyngeal biopsy indicated caseous-follicular tuberculosis (Figure 2), while examination of the excised lymph node revealed caseous-follicular tuberculous adenitis.
Therapeutic interventions: the patient was treated with anti-tubercular antibiotics for 6 months. Combining rifampicin, isoniazid, pyrazinamide, and ethambutol for two months, followed by a four-month course of rifampicin and isoniazid.
Follow-up and outcome of interventions: the clinical progression was characterized by persistent cervical lymphadenopathy, leading to a three-month extension of her treatment. After 9 months of anti-bacillary treatment. The follow-up nasofibroscopy demonstrated regression of her nasopharyngeal process, along with clinical improvement evidenced by the regression of cervical lymphadenopathy.
Patient perspective: I was handicapped by the nasal obstruction, more prominent on the right side, and anxious about the cervical lymphadenopathy. Upon receiving the results of the histopathological study of both biopsies, I felt relieved, as I was afraid of having a malignant tumor of the nasopharynx. After 9 months of antibacterial treatment, I am very satisfied with the regression of cervical lymphadenopathy and the improvement in clinical symptoms.
Informed consent: the patient gives his approval for the publication.
Observation 2
Patient information: a 51-year-old female patient with no significant medical history presented with chronic rhino pharyngitis associated with a one-year history of sleep apnea syndrome.
Clinical findings: on general examination, the patient in good general condition, with stable hemodynamics and respiration. Rhinological examination revealed an inflamed mucosa, associated with nasal obstruction. Nasofibroscopy revealed a bulging of the posterior wall of the nasopharynx.
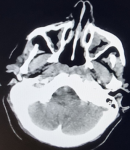
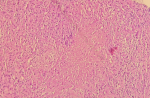
Diagnostic and assessment:a CT scan showed symmetrical and regular thickening of the nasopharyngeal walls without significant pathological enhancement, likely related to adenoid vegetation (Figure 3). Multiple nasopharyngeal biopsies were performed. Histologically, the mucosa was lined by a pseudo stratified columnar epithelium of regular respiratory type. The stroma showed epithelioid and giant-cell granulomas, sometimes centered by areas of necrosis suggestive of caseous necrosis (Figure 4).
Therapeutic interventions: the patient underwent a six-month treatment regimen involving anti-tubercular antibiotics. This included a two-month period of combined rifampicin, isoniazid, pyrazinamide, and ethambutol, followed by a four-month course of rifampicin and isoniazid.
Follow-up and outcome of interventions: clinical evolution was marked by improvement of clinical symptoms. The follow-up nasofibroscopy revealed a reduction in nasopharyngeal bulging.
Patient perspective: I was handicapped by the chronic rhinopharyngitis associated with sleep apnea syndrome. Being with my family me anxious and uncomfortable. I noticed a difference after the treatment. The difference was significant.
Informed Consent: the patient give his approval for the publication.
Tuberculosis (TB) is an infectious disease caused by mycobacterium tuberculosis. Although it primarily affects the lungs (pulmonary TB), it can also manifest in other parts of the body (extra pulmonary TB) [1]. Nasopharyngeal tuberculosis is a rare form of extra pulmonary TB, accounting for less than 1% of TB cases affecting the upper respiratory tract [2]. Nasopharyngeal localization was first described by GRAFF in 1936 [3]. It mainly affects young adults aged 20 to 40 years, with no gender distinction [3]. TB is mainly transmitted through direct airborne transmission, by inhaling particles contaminated with the bacillus from an individual with active pulmonary TB [4]. Less frequently, transmission can occur through hematogenous or lymphatic spread from a local tuberculous infectious focus. Exceptionally, contamination can also occur through ingestion of raw milk contaminated with bovine bacillus [4]. Nasopharyngeal tuberculosis typically presents as a pseudo-tumoral form, with clinical signs similar to those of nasopharyngeal carcinoma [3]. The main symptoms include lymphadenopathy, rhinological symptoms with nasal obstruction and/or epistaxis, as well as otological symptoms presenting as seromucous otitis. Additionally, a general state of malaise is often present [4,6].
The definitive diagnosis is established by histology, which reveals the presence of epithelioid and giant-cell granulomas accompanied by caseous necrosis [4,5]. The endoscopic examination of the nasopharynx can reveal different types of lesions: ulceration, irregular bulging of the nasopharynx, regular mucosal hypertrophy, and sometimes a typical appearance of adenoid vegetation [7]. Since December 2010, WHO has approved the introduction of new tools, mainly in molecular biology, including the Xpert/MTB/Rif or GeneXpert® test, which has increased sensitivity and shortened the confirmation time for TB [8]. This test is also used to detect rifampicin resistance [8]. The main differential diagnosis is nasopharyngeal carcinoma, particularly undifferentiated carcinoma of the nasopharynx (UCNT), which is very common in the Moroccan population [9]. Other differential diagnoses include sarcoidosis, Wegener's granulomatosis, syphilis, and leprosy [10]. The therapeutic management of nasopharyngeal tuberculosis is based on a medical approach using a combination of anti-bacillary antibiotics. The typical treatment protocol involves a combination of Rifampicin (10mg/kg/day), Isoniazid (5mg/kg/day), Ethambutol (15 mg/kg/day), and Pyrazinamide (20 to 30 mg/kg/day) for two months, followed by a continuation phase of rifampicin and pyrazinamide for four months [8]. Treatment efficacy is evaluated by monitoring the regression of clinical and endoscopic signs. Any abnormal evolution should raise suspicion of treatment resistance or the possibility of coexisting neoplastic disease, warranting the need for iterative biopsies [7]. Generally, the prognosis is almost always favorable. The few cases of failure (approximately 1%) are usually due to the emergence of Mycobacterium tuberculosis strains resistant to anti-tuberculosis drugs [10].
Nasopharyngeal tuberculosis is a rare but significant condition to recognize. It presents diagnostic challenges due to its similarity to neoplastic pathologies. Diagnosis is primarily based on histopathological analysis. Treatment involves anti-bacillary drug therapy. The prognosis with anti-bacillary treatment is generally good, with treatment failure mainly attributed to the emergence of multi-drug resistant strains.
The authors declare no competing interests.
Anouar Ben Ameur El Youbi described the case, did a literature search, and wrote the first draft of the manuscript. Mariam Ameziane Hassani reviewed the manuscript and made a substantial contribution. Abdellatif Oudidi reviewed the description of the case and did a concurrent literature search. Nawal Hammas was involved in the histopathological study. All the authors have read and agreed to the final manuscript.
Figure 1: axial CT scan showing irregular and extensive tissue thickening of the postero-lateral walls of the nasopharynx, largely obstructing the rhinopharyngeal lumen
Figure 2: histological image depicting the nasopharyngeal mucosa with a granulomatous lesion centered on caseous necrosis (HESx100)
Figure 3: an axial CT scan image showing symmetrical and regular thickening of the nasopharyngeal walls
Figure 4: histological image displaying an epithelioid granuloma with caseous necrosis (HESx200)
- WHO. Global tuberculosis report 2014.
- Nieves CS, Onofre RD, Aberin-Roldan FC, Gutierrez RL. Nasopharyngeal tuberculosis in a patient presenting with upper airway obstruction. Philippine Journal of Otolaryngology Head and Neck Surgery. 2010 Jun 16;25(1):20-2. Google Scholar
- Tse GM, Ma TK, Chan AB, Ho FN, King AD, Fung KS et al. Tuberculosis of the nasopharynx: a rare entity revisited. Laryngoscope. 2003 Apr;113(4):737-40. PubMed | Google Scholar
- Ndadi Tchiengang KJ, Senghor F, Kane Y, Sagna J, Diatta A, Diom ES. Tuberculose Faciale à Double Localisation: Nasopharyngée et Nasosinusienne: À Propos d´un Cas. Health Sciences And Disease. 2020 Sep 8;21(9). Google Scholar
- Hmidi M, Elboukhari A, Touiheme N, Kettani M, Rguibi M, Messary A. Tuberculose nasosinusienne avec extension cutanée: à propos d'un cas. La Lettre du pneumologue. 2011;14(3):106-8. Google Scholar
- Bouaity B, Nadour K, Hemmaoui B, Errami N, Benariba F, Aljalil A. Tuberculose du naso-pharynx: à propos d'un cas. La Lettre d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2009;(319):14-16. Google Scholar
- Hadid F, Oulghoul O, Benjelloun H, Benhommad O, Raji A, Rochdi Y. Nasopharngeal Tuberculosis Simulating Cancer: About 2 Cases. European Journal of Medical and Health Sciences. 2021 May 28;3(3):46-8. Google Scholar
- llé S, Boubé DA, Bako ID, Timi N, Ganda Aissa M, Dan Sono A. A rare case of cavum tuberculosis. J Func Vent Pulm. 2021;36(12):64-67. Google Scholar
- Oudidi A, Hachimi H, Alami MN. Tuberculose du cavum. J Otolaryngol. 2007 Aug;36(4):253-5. Google Scholar
- Touati MM, Darouassi Y, Chihani M, Lakouichmi M, Tourabi K, Ammar H, Bouaity B. La tuberculose extra-ganglionnaire primitive de la sphère ORL: à propos de 15 cas [ENT primitive extranodal tuberculosis: about 15 cases]. Pan Afr Med J. 2014 Oct 21;19:179. Google Scholar